DANIL HAMMOUDI.MD

ANAT:
|
|
|
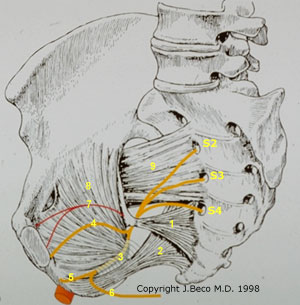
Right
gluteal region
Nerve supply to perineum
The nerve supply to the perineum
originates from three main sources: 1. The Genito-femoral
Nerve (L1,L2). 2. The pudendal
nerve arises from the anterior rami of the second to fourth sacral
roots. These form a trunk before leaving the pelvis via the greater sciatic
foramen. It passes immediately behind the ischial spine and swings forward to
enter the perineum via the lesser sciatic foramen. The nerve passes through
the ischiorectal fossa where it gives off its terminal branches. The inferior
rectal nerve innervates the external anal sphincter and the perianal skin.
The perineal nerve innervates the sphincter urethrae and other muscles of the
anterior compartment via a deep branch, and the skin of the perineum poterior
to the clitoris via its superficial branch. The dorsal nerve of the clitoris
supplies the skin surrounding this structure. 3. The perineal
branch of the posterior femoral nerve. Pudendal Nerve Block
|
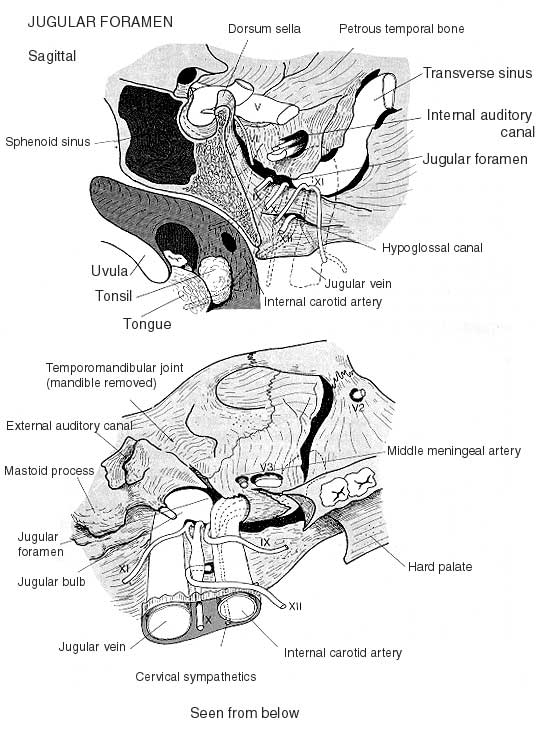
- A TUMOR IN THE RIGHT JUGULAR FORAMEN =č SHOULDER DROOPč PATRALYSIS OF THE TRAPEZIUS MUSCLE INNERVATED
PAR XI
THREE CRANIAL NERVE GO
THROUGH THIS FORAMEN:
- -IX
[GLOSSOPHARYNGEAL NERVE]
- -X
[VAGUS NERVE]
- -XI
[SPINAL ACCESSORY NERVE]
- JUGULAR VEIN EXIT THIS FORAMEN
X + IX ==č DYSPHAGIA + HOARSENESS

Upper
extremity:
Cephalic and Basilic veins are the superficial veins of the arm.
Basilic vein is the largest arm vein measuring 6 – 8 mm. Its course is along
the medial (ulnar) aspect of the arm from wrist to shoulder. It begins at the
dorsum of the hand, crosses the elbow and drains into the brachial vein.
Cephalic vein, measuring 4 – 6 mm, runs along the lateral (radial)
aspect of the arm also from the wrist to shoulder emptying into the axillary
vein.
Although the basilic vein is larger, the
cephalic vein is more superficial and easier to dissect out. Therefore it is
often the preferred vein for dialysis fistulas or grafts.
Conversely, the cephalic vein may take an
acute angle before it enters the axillary vein sometimes making negotiation
with a catheter or wire difficult.
Both
veins are good access for:
a. peripheral IV's
b. PICC lines
c. arm ports
Median
vein:
Forms
a Y just below the elbow and drains into both the basilic and cephalic veins.
Median
antecubital vein:
Oblique
coursing vein at the elbow that joins the basilic and cephalic veins.
Deep
forearm veins:
These
are 2 or 3 veins each that course with and are named like the corresponding
arteries of the forearm (radial & ulna).
Brachial veins are the deep veins of the upper arm, usually
paired and smaller than the superficial veins. They travel in the upper arm
parallel to (on either side) the brachial artery and join with the basilic vein
to form the axillary vein.
Brachial
veins can be used for:
a. PICC lines
b. arm ports
Although
not universal, many attempt placement of long term venous access between the
elbow and the shoulder when using upper extremity veins. This avoids catheter
irritation and compression from repetitive flexion at the elbow
Lower extremity:
Femoral
Vein:
The
femoral vein is the continuation of the popliteal vein beginning at the adductor
hiatus. It receives the greater saphenous vein and the deep femoral vein. It
continues as the external iliac vein at the inguinal ligament.
It
usually lies posterolaterally to the femoral artery in the thigh and then moves
medially at the groin. In approximately 25% of people the femoral vein is
directly posterior to the artery at the groin.
Traditionally,
femoral veins are not routinely used for venous access except on an
acute temporary basis or when all other sites have been exhausted.
Theoretically,
the proximity to the groin increases the likelihood of contamination and
infection. In addition, this location predisposes to catheter kinking and
significantly affects ambulation.
Moreover,
like other venous access sites, femoral catheters can cause thrombosis. The
consequences of thrombosis may have greater clinical significance
in the larger, dependent, lower extremity.
Despite
these caveats, we have begun using this site for dialysis access in those
patients with severely limited access and have had reasonable success.
Femoral
vein access – potentially more contamination and symptomatic DVT.
Chest and Neck:
Axillary Vein:
The
axillary vein begins at the junction of the basilic and brachial veins. It runs
medial, anterior and caudal to the axillary artery, to the lateral border of
the first rib where it becomes the subclavian vein.
It
lies caudal to the lateral half of the clavicle, slightly medial to and partly
overlies the axillary artery. The artery and vein are within the axillary
fascia. The brachial plexus (nerves) runs between artery and vein.
Valves
may be present near the junction of the brachial and basilic veins.
Axillary
vein access can be utilized to "prevent pinch off syndrome". This
results from the more classical medial subclavian vein approach for central
venous access (see complications for more information). If done from a lateral
approach with sonography, axillary vein access can also decrease the incidence
of pneumothorax.
The
down side is that this approach, however, is that it still may incite the same
amount of stenosis and thrombosis as the subclavian approach.
Subclavian
Vein:
The
subclavian vein runs from the lateral border of the first rib to the sternal
end of the clavicle where it joins the internal jugular vein and becomes the
brachiocephalic vein.
It
lies posterior and superior to the subclavian artery.
A
pair of valves is not uncommon at the termination of the subclavian vein.
The
subclavian vein becomes the axillary vein at the lateral margin of the first
rib.
The
thoracic ducts enter the superior aspect of the subclavian vein near its
junction with the internal jugular vein.
Access
can be achieved via the anatomical landmark approach or with imaging. Using
landmarks, an access needle is advanced medially along a horizontal plane
beneath the medial 2/3’s of the clavicle towards the suprasternal notch of the
manubrium.
As
detailed under the procedure section, it is safer and more accurate
to use imaging. In the case of the subclavian vein, venography or
ultrasound can be utilized. Imaging permits a more lateral approach (axillary
vein) which decreases the chance for pneumothorax and catheter compression from
pinch
off syndrome.
Additionally,
structures such as the Phrenic nerve, brachial plexus and pleural cupola all
lie within close proximity to the subclavian vein.
Subclavian
vein access is predisposed to both acute and chronic complications. (see complications)
We
avoid this approach unless absolutely necessary.
In
one report, using dialysis catheters, the complication rate for subclavian vein
access was 44.2% higher than the internal jugular vein route. Anatomically, the
right jugular provides a straight shot to the right atrium. The right
subclavian approach forces the catheter to abut up against multiple 'pressure
points' in the vein. In theory, the constant irritation from the catheter
at these points could result in intimal hyperplasia and possibly explain the
early failure of the sublavian access reported in the literature.
The
pneumothorax rate is also higher from this approach as compared with the
internal jugular vein. In addition, the infection rate for the subclavian vein
route was more than twice the internal jugular vein.
Axillary
and subclavian veins can be used for:
a. PICC line
b. Non-tunneled CVC
c. Tunneled CVC
d. Chest ports
Internal jugular vein (IJ):
The
internal jugular vein exits the jugular foramen of the skull base and courses
inferiorly along with the carotid artery and vagus nerve The IJ begins posterior
to the carotid artery at the cranium but spirals around the artery and ends up
anteriorly at the level of the chest. It lies between the two heads of the
sternocleidomastoid muscle in the mid portion and finally lies posterior to the
clavicular head of the muscle. It joins with the subclavian vein to become the
brachiocephalic vein.
The
IJ, especially the right side has become the preferred site for long term
CVC’s.
Reasons
for (R) IJ preference for CVC’s:
a. superficial position
b. large size
c. high flow
d. greater distance from the lung
e. straight course to the SVC (catheter
less likely to irritate venous endothelium)
f. less malposition
g. less stenosis and occlusion as opposed
to the subclavian vein
f. direct compression of adjacent artery
is easier if inadvertently punctured
Specifically
in dialysis patients, internal jugular vein use protects the subclavian vein
from catheter induced stenosis and occlusion which would preclude shunt
placement on that side.
Percutaneous
puncture of the subclavian and internal jugular vein was popularized by
Stellato et al.
There
are numerous anatomical landmark techniques for accessing the IJ. Commonly the
carotid artery is manually displaced medially and a needle puncture is made
midway between the angle of the mandible and superior margin of the clavicle
directed towards the ipsilateral nipple.

Normally
the IJ vein lies lateral and slightly anterior to the carotid artery.
Because
the course of jugular vein changes, the anatomic relationship between the IJ
and common carotid artery is extremely variable. In addition the IJ may be
small or thrombosed. Therefore, it is best to avoid potential complications by
utilizing sonography for both the pre operative jugular vein assessment as well
as direct visualization during the puncture.
Denys
and Uretsky evaluated 200 consecutive patients with sonography and found that
the IJ was normal size and position in 92%, non-visualized in 2.5%, and
exceedingly small in 3%. Other studies including our own suggest that IJ
variations from normal can occur in up to 28%.
Remember,
variability among authors may relate to the level and degree of neck rotation
when examined with ultrasound. As the neck is turned away from 30 to 90 degrees
the IJ assumes a more anterior position in relation to the carotid artery.
The
Valsalva maneuver or Trendelenburg position can increase the size of the IJ. If
these maneuvers do not increase the IJ size, distal stenosis or obstruction
should be considered.
Another
caveat - extending the patient’s neck may actually flatten and decrease the
size of the IJ vein.
When
using ultrasound, the transducer orientation should be transverse to clearly
differentiate between carotid artery and IJ.
The
anatomic relationship of the internal jugular vein to the carotid artery
varies. Sonography lessens the complications of inadvertent puncture and or
cannulation of the carotid artery.
Variable relationship of Internal Jugular Vein and
Carotid Artery

External
jugular (EJ):
The
external jugular vein (EJ) begins approximately at the level of the angle of
the mandible (from the junction of the posterior auricular and the
retromandibular veins) and courses posterior to the sternocleidomastoid muscle
to enter inferiorly into the subclavian vein.
Occasionally
both the IJ and EJ may have incomplete or valve like structures.
Two
sets of valves, tortuosity and course make the EJ less useful for venous
access. Also, some EJ veins terminate in more of a plexus making catheter
traversal difficult.
Some
authors suggest that although it is not the most reliable route it is the
safest.
Intercostal veins:
There
are both anterior and posterior intercostal veins. The posterior division
enters into the azygous and hemiazygous systems. The anterior division empties
into the internal mammary vein. They lie beneath the ribs and serve as a
collateral pathway in the presence of central deep venous thrombosis (DVT). As
collaterals they may hypertrophy and be accessible for venous access.
Complications
of access include PTX and damage to the neurovascular bundle.
Use
of the external jugular and intercostal veins depends on their size.
a. PICC lines
b. Occasionally non-tunneled central
lines
c. Rarely tunneled catheters
Abdomen:
Inferior
vena cava (IVC):
The
IVC is formed from the junction of the common iliac veins at
approximately the L5 level. It courses upwards towards the heart anteriorly and
to the right of the spine. It lies to the right of the aorta and is oval in
shape.
The
renal veins enter the IVC at approximately the lower third of L1. The left
renal vein enters slightly higher than the right. Both can be duplicated. IVC duplication .2%,
Left renal vein duplication 11- 17%.
The
IVC is commonly used for CVC’s when other sites are exhausted. It can be used
for essentially any type of CVC but mostly for long term tunneled catheters.
Considering the position of the IVC, be sure the CVC length is adequate.
The
IVC can be accessed by either the translumbar or the transhepatic route.
Hepatic
veins :
These
consist of a right, middle and left. All three may join and enter the IVC as a
common trunk but most commonly the right enters by itself and in 80% the middle
and left hepatic veins have a common trunk.
The
middle hepatic vein lies in the interlobar fissure separating the R and L lobes
of the liver. The anterior course permits peripheral access.
Caudate
veins (usually 2-3) drain separately into the IVC, several cm’s below the main
hepatic veins.
Like
the IVC the hepatic veins are recognized as a last resort type of access site.
The middle hepatic vein is the most commonly chosen. It is most anterior
and can provide a long intravascular course. This helps eliminate migration
(withdrawl) of the catheter that occurs with respiration.
Any
type of CVC can be placed.
Most
prefer a subcostal approach to help avoid pneumothorax. Ultrasound can be
utilized for localization and guidance if preferred. Once the hepatic vein is
cannulated a guide wire is advanced to the IVC. The tract is serially dilated
and a peel away sheath placed. As with other methods the catheter and tunnel
length are determined and the catheter tip placed in the lower right atrium.
We
also prefer the subcostal approach and use ultrasound to localize a hepatic
vein. After appropriate patient preparation and local anesthesia we use an antegrade
approach.
We
connect a 10 cc syringe of diluted contrast to a 22 ga. Chiba needle and
advance the needle towards the localized vein while injecting small volumes of
contrast approximately every 0.5 cm. Using fluoroscopy, the hepatic vein is
opacified and cannulated. This method also allows for needle redirection if a
vital structure is transgressed. As before, we also "test the tract"
before proceeding with catheter placement.
In addition,
unless a specific catheter is required, we use a small (6 Fr.) self retaining
catheter to avoid migration.
The
major problem with this approach is catheter migration from normal respiratory
motion.
Hepatic
vein thrombosis has not been a clinical problem.
Infections
unique to this approach have not been reported.
Collateral Veins:
Collaterals
form in response to more centrally occluded veins. Their purpose is to re-route
blood back to the right atrium. They can occur anywhere but are common in the
chest and neck. Because of their diminutive size and tortuous course they are
usually best for PICC lines, however, small tunneled and non-tunneled lines are
a possibility.
Collaterals
are especially useful in individuals with a coagulopathy where other sites are
more prone to bleeding.
Common
collaterals employed include intercostal and chest wall veins.
When
choosing a collateral vein for central venous access, it is important to be
sure that it is not the last remaining draining vein in the event that it also
becomes thrombosed.
Thrombosed
Veins:
Many
long-term central venous access patients have limited access due to thrombosis
of previous sites. In these individuals it may be feasible to preserve the
remaining access sites by negotiating through obstructed veins either for
reconstruction of the vein or simple placement of a catheter.
Although
these veins appear impenetrable, using sonography, guide catheters, hydrophilic
guide wires and time, many can be negotiated. Once the occlusion is bypassed,
the vein can be dilated using tapered Teflon dilators, Van Andel or balloon
catheters. Occasionally, the CVC may be simply placed through the occlusion
without dilatation.
Because
these vessels have become essentially useless, complications are rare and if
negotiation is unsuccessful, nothing is lost. Perforation is rare and often
clinically inconsequential, however, proper technique should be employed to
prevent this.
The
following is a technique that we find helpful in those chronic obstructions
that allow passage of a guide wire but are so firm that they preclude traversal
by a catheter.
First
gain access from above as usual and negotiate a wire through the obstruction.
Next gain access from below, i.e. femoral vein, and snare the wire that has
been negotiated through the obstruction.
Next,
place a dilator or tapered catheter over the guide wire from above and hemostat
the wire just distal to the catheter hub. Now, pull the catheter through the
occlusion by pulling the wire from the femoral access.
Thrombosed
vein access can be used for all types of CVC’s.
- deep fascia of neck condenses to form four layers: investing, pretracheal, prevertebral, and carotid sheath
Investing Layer
- surrounds neck like collar
- splits to enclose two muscles (trapezius
& sternocleidomastoid), two salivary glands (parotid &
submandibular) and two spaces (suprasternal & supraclavicular)
- between angle of mandible and mastoid process,
it splits into two laminae to enclose parotid gland, superficial lamina (parotid fascia) extends to zygomatic arch
- deeper lamina (between angle of mandible and
styloid process) forms stylomandibular ligament
- forms roof of anterior and posterior triangles
of neck
Attachments
- sup: ext. occipital protuberance, sup nuchal
line, mastoid process, lower border of mandible
- inf: spine of scapula, acromion process,
clavicle, manubrium
- post: ligamentum nuchae, C7
- ant: symphysis menti, hyoid bone
Pretracheal
Fascia
- lies deep to infrahyoids
- splits to enclose thyroid, trachea and
oesophagus
Attachments
- sup: hyoid bone, thyroid cartilage, cricoid
cartilage
- inf: fibrous pericardium
- lat: ant layer of carotid sheath
Prevertebral
Fascia
- situated in front of prevertebral muscles of
neck (surrounds cervical vertebrae and associated muscles)
- forms floor of post. triangle of neck
- cervical and prox. brachial plexuses are deep
to this fascia
- axillary sheath is extension of this fascia
Attachments
- sup: base of skull
- inf: body of T4
- inf & lat: axillary sheath
Carotid Sheath
- encloses common carotid and internal carotid
arteries, internal jugular vein, and vagus nerve
- ansa cervicalis embedded in ant wall
- sympathetic chain lies post, outside sheath
- runs from base of skull to sup mediastinum
- junctional area between neck and thorax
- key structures: thoracic
inlet, cervical pleura, scalenus anterior
- oval shaped (transverse > A-P)
- plane: oblique (post higher than ant)
Boundaries
- post: T1
- lat: 1st ribs and costal cartilages
- ant: manubrium sterni
Contents
Arteries
- right (r): brachiocephalic trunk, branches into
r. subclavian and r. common carotid
- left (l): l. subclavian, l. common carotid
Brachiocephalic
Trunk
- largest branch of arch of aorta, 4-5 cm in
length and arises post to centre of manubrium
- passes sup and to right, post to
sternoclavicular joint where it divides into r. subclavian a. and r.
common carotid a.
- covered by sternohyoid and sternothyroid
muscles
Subclavian
- is divided into three parts by scalenus
anterior, it gives the following branches:
- Part 1 (med): vertebral, internal thoracic,
thyrocervical trunk ( inf. thyroid, transverse cervical,
suprascapular)
- Part 2 (post): costocervical trunk (
sup intercostal, deep cervical)
- Part 3 (lat): dorsal scapular, (occasionally
suprascapular a)
Veins
- subclavian (from axillary v.), anterior to
scalenus anterior
- internal and anterior jugular vv.
Anterior
Jugular
- smallest of jugular veins, usually paired
(joined by jugular venous arch just sup
to sternum)
- arises near hyoid from confluence of
submandibular veins (submental venous plexus)
- descends in superf fascia between mid line and
ant sternocleidomastoid, turns lat at root of neck and opens into
termination of ext jugular
Nerves
- phrenic n. (lat.)
- vagus + recurrent laryngeal
- sympathetic chain (med.)
Vagus
- leaves skull through jugular foramen with
internal jugular vein and CN IX and XI
- descends in the carotid sheath
- on right: vagus crosses origin of subclavian a.
(post to brachiocephalic vein) and gives off recurrent
laryngeal n. which loops back around subclavian
- on left: recurrent
laryngeal n. given off to loop around arch of aorta
- after looping both recurrent laryngeal nn.
ascends to reach inf pole of thyroid where they ascend in tracheoesophageal groove to supply all intrinsic
muscles of larynx except cricothyroid
Phrenic Nerve
- sole motor nerve to diaphragm
- it arises from C3,4,5 nerves
- it descends obliquely across the ant surface of
scalenus ant, deep to prevertebral fascia
- crosses between subclavian v and a.. to enter
thorax
Sympathetic
Chain
- has three enlargements (ganglia), superior, middle, inferior
- inf: lies at sup 1st rib, wrapped
around vertebral a., usually fused with 1st thoracic ganglion
- mid: lies on ant aspect of inf thyroid a.
around level of cricoid cartilage (C6 vertebra)
- sup: located at level of atlas and axis, large
(2-3 cm long)
Lymphatics
- left: thoracic duct
- right: r. lymphatic duct receives jugular,
subclavian and bronchomediastinal lymph trunks
Viscera
- trachea
- oesophagus
- apex of lung with dome of pleura
Muscles
- longus colli
- sternal ends of sternocleidomastoid,
sternohyoid, sternothyroid
- scalene muscles
Ligament
- ant. longitudinal lig.
- triangular area in neck enclosed between sternocleidomastoid and
trapezius
Boundaries
- base: mid 1/3 of clavicle
- apex: lies on sup. nuchal line
- ant: post border of sternocleidomastoid
- post: ant border of trapezius
- roof: investing layer of cervical fascia
- floor: prevertebral fascia fascia covering
splenius capitus, levator scapulae, scalenus medius, and scalenus
posterior
Contents
- nerves: spinal accessory, cervical plexus (including
phrenic), brachial plexus
- accessory n. (CN XI) divides post triangle into
sup and inf parts, runs between sternocleidomastoid and trapezius
(supplying both), enters at 1/3 way down sternocleidomastoid
- lesser occipital n. (C2) ascends short distance
along sternocleidomastoid before it divides to supply skin of neck and
scalp post to auricle, and sup auricle
- greater auricular n. (C2-3) curves over post
sternocleidomastoid, supplies branches to skin of neck, divides into ant
& post branch to supply inf auricle, and area from mastoid to
mandible
- transverse cervical n. (C2-3) curves around the
post border of sternocleidomastoid near its middle, passes transversely
across it, supplies skin of ant triangle of neck
- supraclavicular nn. (C3-4) arise as single
trunk, which divides into med, intermediate and lat branches
- phrenic n. (C3-5) curves around lat border of
scalenus ant, descends obliquely across ant surface, deep to transverse
cervical and suprascapular aa., enters thorax by crossing origin of
internal thoracic a. between subclavian a. & v.
- arteries: subclavian (3rd
part), transverse cervical, suprascapular, occipital
- veins: external jugular, (subclavian)
- pierces and fuses with investing cervical
fascia about 5 cm above clavicle
- if cut fascia prevents it from closing and can
cause intravenous air embolus
- lymph nodes
- muscles
|
Muscle |
Origin |
Insertion |
Innervation |
Action |
|
Splenius capitus |
inf ligamentum nuchae, spinous processes
of T1-T6 |
lat mastoid process and sup nuchal line |
cervical spinal nn. |
lat flexes head & neck, rotates head
& neck to same side |
|
Levator scapulae |
transverse processes of C1-C4 |
sup med scapula |
cervical spinal nn. |
elevates scapula |
|
Scalenus posterior |
transverse process of C4-C6 |
2nd rib |
cervical spinal nn. |
lat flexes neck, elevates 2nd
rib |
|
Scalenus medius |
transverse process of C2 & C7 |
sup post 1st rib |
cervical spinal nn. |
lat flexes neck, elevates 1st
rib |
|
Sterncleidomastoid |
2 heads, sternal and clavicular |
lat mastoid process, lat sup. nuchal line |
CN XI |
extend atlantio-occipital joint, flex
cervical vertebrae |
Subdivisions
- inf belly of omohyoid splits
post triangle into large occipital
triangle and small
supraclavicular triangle
- occipital: occipital a. appears in its apex,
contains important accessory n.
- supraclavicular: location indicated on neck by
supraclavicular fossa, crossed by subclavian a. and external jugular v.
- anterior triangle =
triangular area on front of neck
Boundaries
- ant: midline
- post: ant border of sternocleidomastoid
- base: lower border of mandible, line drawn from
angle of mandible to mastoid process
- apex: jugular notch
Contents
- muscles:
- suprahyoid muscles: mylohyoid
(floor of mouth), geniohyoid (reinforce
floor of mouth), stylohyoid (small slip on
each side), digastric (straplike, two
bellies, intermediate tendon joined to hyoid)
- infrahyoid muscles: omohyoid
(two bellies, intermediate tendon joined to clavicle), sternohyoid (superf, except inf), sternothyroid (deep to sternohyoid), thyrohyoid (sup continuation of sternothyroid)
|
Muscle |
Origin |
Insertion |
Innervation |
Actions |
|
Mylohyoid |
mylohyoid line of mandible |
hyoid |
mylohyoid n. (branch of V3 n.) |
elevates hyoid, floor of mouth and tongue |
|
Geniohyoid |
inf mental spine of mandible |
hyoid |
C1 n |
pulls hyoid ant-sup, shortens floor of
mouth, widens pharynx |
|
Stylohyoid |
styloid process |
hyoid |
facial n. |
elevates and retracts hyoid |
|
Digastric |
ant belly: mandible post belly: mastoid process |
intermediate tendon: hyoid |
ant belly: mylohyoid n. post belly: facial n. |
depresses mandible, raises and steadies
hyoid |
|
Omohyoid |
Sup border of scapula |
hyoid |
ansa cervicalis |
depresses, retracts and steadies hyoid |
|
Sternohyoid |
manubrium and med clavicle |
hyoid |
ansa cervicalis |
depresses hyoid |
|
Sternothyroid |
post surface ofmanubrium |
thyroid cartilage |
ansa cervicalis |
depresses hyoid and larynx |
|
Thyrohyoid |
thyroid cartilage |
hyoid |
C1. |
depresses hyoid and raises larynx |
- arteries: common
carotid, internal carotid, external carotid + branches
- veins: ant
jugular, int jugular + tributaries
- nerves: (IX), X,
XI , XII, ansa cervicalis, sympathetic trunk
- viscera: pharynx, oesophagus, larynx, trachea
- glands: parotid, submandibular, thyroid, parathyroid
- submandibular fills most of digastric triangle,
submandibular duct (5 cm) passes from deep
process of gland to open on sublingual papilla
Subdivisions
- sup belly of omohyoid and
digastric muscles subdivide anterior triangle into four smaller triangles: submental, digastric, carotid, and muscular
|
|
|
Submental |
Digastric |
Carotid |
Muscular |
|
Boundaries |
|
median triangle situated between ant bellies of digastric
muscles and hyoid bone floor: mylohyoid muscle |
ant: ant digastric post: post digastric sup (base): base of ant triangle floor: mylohyoid, hyoglossus, part of mid constrictor of pharynx |
ant-inf: sup omohyoid post: ant sternocleidomastoid sup: post digastric & stylohyoid floor: thyrohyoid, hyoglossus, mid & inf constrictors of pharynx |
bounded by ant sternocleidomastoid, sup
omohyoid, median plane floor: infrahyoid muscles |
|
Contents |
Arteries |
|
facial vessels mylohyoid vessels submandibular vessels carotid sheath + contents |
common carotid int & ext carotid + branches (sup
thyroid, asc pharyngeal, lingual, facial, occipital, post auricular) |
|
|
Veins |
submental |
int jugular + tributaries (facial,
pharyngeal, lingual, sup & mid thyroid) |
|
||
|
Nerves |
|
mylohyoid nerves CN IX, X, XII |
CN IX, X, XI ansa cervicalis sympathetic chain |
ansa cervicalis |
|
|
Muscles |
|
hyoglossus mylohyoid |
|
infrahyoid muscles (sternohyoid, omohyoid,
sternothyroid, thyrohyoid) |
|
|
Other |
submental lymph nodes |
submandibular gland lower part of parotid gland |
deep cervical lymph nodes carotid body |
neck viscera |
|
|
Notes |
|
|
|
carotid sinus (baroreceptor) dilation of
prox int carotid a., innervated by sinus branch of glossopharyngeal carotid body lies (chemoreceptor) lies
behind, also supplied by sinus branch best site to approach big blood vessels in
neck |
all infrahyoids supplied by ansa
cervicalis, except for thyrohyoid, supplied by C1 |
- between infrahyoid muscles are number of structures in and
adjoining midline of neck
- hyoid bone
- median thyrohyoid ligament
- laryngeal prominence
- cricothyroid ligament
- cricoid cartilage
- cricothyroid muscle
- first tracheal ring
- isthmus and pyramidal lobe of thyroid
- inferior thyroid veins
- jugular venous arch (joins two anterior jugular
vv.)
- thyroid ima a.
Arteries
Common Carotid
Arteries
- r. common carotid begins at bifurcation of
brachiocephalic, l. arises from arch of aorta (post to sternoclavicular
joints)
- ascends within carotid sheath to level of sup
border of thyroid cartilage where it terminates by dividing into int
& ext carotid aa.
Internal
Carotid Artery
- has no branches in neck, but are two of four
major aa. that supply blood to brain
- each passes vertically upwards from common to
enter carotid canal in petrous part of
temporal bone, accompanied by plexus of sympathetic fibres
- during course through neck, lies deep to
sternocleidomastoid m and parotid gland
- enters middle cranial fossa through the
superior part of foramen lacerum
- supplies pituitary, orbit and most of
supratentorial part of brain
External
Carotid Artery
- extends between C3/C4 vertebra to the neck of
the mandible
- runs midway between mastoid process and angle
of mandible within the parotid gland
- terminates by dividing into
two branches, maxillary a. and superficial
temporal a.
Branches of
External Carotid Artery
|
Surface |
Branch |
Notes |
|
Anterior |
superior thyroid |
arises close to origin of ext carotid,
just inf to greater horn of hyoid runs ant-inf (deep to infrahyoids) to
reach sup pole of thyroid also gives off muscular branches to
sternocleidomastoid and infrahyoid muscles, and sup
laryngeal a. |
|
Lingual |
arises from ext carotid where it lies on
mid constrictor of pharynx arches sup-ant at the level of greater
horn of hyoid) and n passes deep to hypoglossal n.,
stylohyoid and post digastric disappears deep to hyoglossus muscle, then
on genioglossus to becomes deep lingual a. |
|
|
Facial |
arise from ext carotid just sup to the
lingual a. gives off tonsillar
branch and branches to palate passes sup (under stylohyoid, digastric
), loops ant and enters deep groove in submandibular gland crosses inf border of mandible and enters
face |
|
|
Posterior |
Occipital |
arises near level of facial a., passes
post along inf border of post belly of digastric, ends in post part of scalp,
during course pass superf to int carotid a. and CN IX, X and XI |
|
post auricular |
arise at sup post belly of digastric,
ascends post of ext auditory meatus and supplies adjacent muscles, parotid
gland, facial n. and scalp |
|
|
Medial |
asc. Pharyngeal |
ascends on pharynx (deep to int carotid)
and sends branches to pharynx, prevertebral muscles, middle ear and meninges |
Veins
Internal
Jugular Vein
- largest vein in neck (usually larger on right
side than left)
- drains blood from brain and superf part of face
and neck
- course corresponds to line drawn from external
acoustic meatus to med end of clavicle
- commences at jugular foramen
in post cranial fossa, as direct continuation of sigmoid sinus, from
dilation at origin (sup bulb of
int jugular v.)
it runs in carotid sheath, leaves ant triangle by passing deep to
sternocleidomastoid and unites with subclavian post to med clavicle
- inf bulb of int jugular v. located near termination, contains bicuspid
valve
- tributaries: petrosal sinus, facial, lingual,
pharyngeal, sup and middle thyroid and often occipital vv.
- largest of endocrine glands
- consists of two lateral lobes, isthmus and occasionally pyramidal
lobe
- isthmus overlies 2nd, 3rd
and 4th tracheal rings
- med lat lobe overlies larynx, trachea,
oesophagus, inf. constrictor of pharynx and cricothyroid muscles
- post surface of lat lobe extends over carotid
sheath
- infrahyoid muscles cover gland anteriorly
- levator glandulae thyroideae attaches pyramidal lobe to hyoid bone,
embryological remnant of thyroglossal duct
- parathyroids are
situated on post border, along line of sup and inf thyroid aa. Anastomoses
- arteries: sup
thyroid a. (from ext carotid a.); inf thyroid a. (from thyrocervical
trunk); and occasionally thyroid ima a.(from arch of aorta).
- veins: sup and
middle thyroid vv.(empty into int jug v); inf thyroid vv (empty into
brachiocephal v)
Clinical
- relation of isthmus to tracheal rings (tracheostomy)
- relation of ext laryngeal n. with sup thyroid a. (ligation of
artery during thyroidectomy, hoarseness of voice because cricothyroid
paralysed)
- relation of recurrent laryngeal n. with inf thyroid a. (ligation of
artery during thyroidectomy, complete loss of voice as n. supplies all
pharyngeal muscles except cricothyroid)
- remnant of thyroglossal duct may give rise to cyst (always located
along ant midline of neck)
- close relationship of parathyroid to thyroid explain development of
hypoparathyroidism is some patients following thyroidectomy
- funnel-shaped fibromuscular tube, common route for air and food
- located post to nasal cavity, mouth and larynx
- divided into three parts: nasopharynx, oropharynx, and
laryngopharynx
- it is about 15 cm in length, extends from base of skull to inf
border of cricoid cartilage
- widest (~5cm) opposite hyoid bone, narrowest (~1.5cm) at inf end
- post wall lies against prevertral fasica, with potential
retropharyngeal space in between
- pharyngeal wall composed of five layers
- mucous membrane
- submucosa
- pharyngobasilar fascia (attached to skull)
- muscular layer composed of inner longitudinal
(stylopharyngeus, palatopharyngeus and salpingopharyngeus) and outer
ciruclar fibres (sup, middle and inf constrictors)
- loose connective tissue layer
forming buccopharyngeal fascia
- supplied mainly by pharyngeal plexus of
nn. (formed by CN IX (sensory) and X (motor)); nasopharynx receives its
sensory supply mainly from CN V3
- air conducting tube, measures ~ 5 cm in length
- located in front of C3-C6 vertebrae below the hyoid bone
- cartilages: 3 single
(epiglottis, thyroid, cricoid); 3 paired (arytenoid, corniculate,
cuneiform)
- membranes and ligaments:
- extrinsic: thyrohyoid membrane, cricotracheal
membrane
- intrinsic: quadrangular membrane (extends
between epiglottis and vestibular folds); cricovocal membrane (extends
between vocal ligament and upper border of cricoid cartilage)
Cavity
- divided into three parts:
- upper (vestibular) part; middle (ventricular)
part: between vestibular and vocal folds; and lower (infraglottic) part
- rima glottidis: is the aperture between the two
vocal folds.
Muscles of the
Larynx
- extrinsic muscles that move the larynx up and
down during deglutition:
- elevators of larynx : digastric, stylohyoid,
mylohyoid, and geniohyoid muscles
- depressors of larynx : sternohyoid,
sternothyroid, and omohyoid muscles
- instrinsic muscles: these are small muscles
that move parts of the larynx on each other, and are particularly
concerned with alterations in the length and tension of vocal folds in
the production of voice, and in changing the size of rima glottidis to
facilitate entry of air to the lungs
Nerves of the
Larynx
- sensory nerve supply (to the mucosa) : above
vocal fold: internal laryngeal nerve vocal fold: recurrent laryngeal
nerve
- motor nerve supply (to intrinsic muscles) :
recurrent laryngeal nerve, except for cricothyroid (supplied by external
laryngeal nerve)
Skull: Checklist of bones, sutures, features,
and foramina
SKULL
Cranium (Brain case ) Facial skeleton
or Neurocranium
or Viscerocranium
Calvaria Cranial base
or Cranial Vault or Base of skull
or Upper part of brain case
|
The 8 Bones of cranium: |
The 14 Bones of facial skeleton: |
(4 single and 2 paired) (2single and 6
paired)
Frontal bone (single) Vomer (single)
Ethmoid bone (single) Nasal bone (paired)
Sphenoid bone (single) Lacrimal bone (paired)
Occipital bone (single) Inferior concha (paired)
Parietal bone (paired) Palatine bone (paired)
Temporal bone (paired) Zygomatic bone
(paired) Maxilla (paired)
Mandible (single=two halves)
Skull
: Exterior Views
1. Norma Verticalis ( Superior View ):
Bones Frontal
Parietals
Occipital (
squamous part )
Sutures : Coronal
Sagittal
Lambdoid
Frontal ( Metopic ) [occasional]
Features: Parietal eminence
Bregma
Lambda
Foramen: Parietal
2. Norma Frontalis ( Anterior View ):
Bones : Frontal
Nasal
Maxilla
Zygomatic
Features : Supercilary arches
Glabella
Nasion
Orbit
Anterior nasal
aperture
Anterior nasal
spine
Foramina:
Infraorbital
Zygomaticofacial
3. Norma Lateralis ( Lateral View ):
Bones : Frontal
Parietal
Sphenoid ( greater wing )
Temporal: (
squamous part , and zygomatic, mastoid and styloid processes)
Occipital
Zygomatic
Maxilla
Features: Pterion
Superior and Inferior temporal lines
Supramastoid crest
Temporal fossa
Infratemporal
fossa
Pterygopalatine fossa
Foramina : External accoustic meatus.
Zygomaticotemporal foramen.
4. Norma Occipitalis ( Posterior view ):
Bones : Parietals
Occipital
Temporal ( mastoid part )
Sutures: Lambdoid
Parietomastoid
Occipitomastoid
Features: External occipital protuberance
Superior nuchal line
Inferior nuchal line
Inion.
5. Norma Basalis ( Inferior View ):
Bones: Maxilla: Palatine processes, alveolar
processes
Palatine: Horizontal plate
Sphenoid: Body,
greater wings, and medial and lateral pterygoid
plates.
Temporal: Squamous, petromastoid, and
tympanic parts
Occipital: Basilar and squamous parts
Features: Incissive fossa
Posterior nasal spine
Pharyngeal tubercle
Pterygoid fossa
Scaphoid fossa
Pterygoid hamulus
Infratemporal crest
Spine of sphenoid
Mandibular fossa
Articular tubercle
Jugular fossa
Styloid process
Occipital condyle
Mastoid process
Mastoid notch (groove for posterior belly of
digastric muscle)
External occipital crest
Superior and inferior nuchal lines
External occipital protuberance
Foramina : Incisive
Greater and lesser palatine
Foramen ovale
Foramen spinosum
Foramen lacerum
Opening for auditory tube
Carotid canal
Pterygoid canal
Foramen magnum
Hypoglossal canal
Jugular foramen
Stylomastoid foramen
Posterior nasal apertures (choanae)
Interior
of the Skull
- Inner aspect of the calvaria (vault)
Bones: Frontal
Parietal
Occipital
Features : Frontal crest
Groove for superior sagittal sinus
Groove for brances of middle meningeal
vessels
Depressions for arachnoid granulations
Foramina: Parietal
B. Cranial Fossae:
- Anterior Cranial Fossa:
Bones: Frontal (orbital plates)
Ethmoid (cribriform plate)
Sphenoid (lesser wings and jugum)
Features: Crista galli
Anterior clinoid process
Foramina: Cribriform plate foramina
Foramen caecum
Nasal slits
- Middle Cranial Fossa:
Bones: Sphenoid (body and greater wings)
Temporal (petrous and squamous parts)
Parietal
Features: Sulcus chiasma
Sella turcica
Tuberculum sellae
Hypophyseal fossa
Dorsum sellae
Posterior clinoid processes
Groove (sulcus) for internal carotid artery
Middle clinoid process
Impression for the trigeminal ganglion
Foramina: Optic canal
Superior orbital fissure
Foramen rotundum
Foramen ovale
Foramen spinosum
Foramen lacerum
Fissures for greater and lesser petrosal
nerves
- Posterior cranial fossa:
Bones: Occipital (basillar and squamous
parts)
Temporal (petrou..s and mastoid parts)
Parietal
Sphenoid (body)
Features: Groove for transverse sinus Groove
for sigmoid sinus
Internal occipital crest
Internal occipital protuberance
Clivus
Foramina: Foramen magnum
Jugular foramen
Hypoglossal (anterior condylar) canal
Internal auditory (acoustic) meatus
Posterior condylar canal
.
Bones
of the orbit
Margins of the orbit:
Medial: Frontal and maxillary bones
Superior: Frontal bone
. Lateral: Zygomatic and frontal bones
Inferior: Zygomatic and maxillary bones
Walls of the orbit:
Medial wall: Maxilla (frontal process)
Lacrimal bone
Ethmoid (orbital part)
Sphenoid (body)
Features: Nasolacrimal canal
Anterior and posterior ethmoid foramena
Roof (Superior) wall: Frontal (orbital
plate)
sphenoid (lesser wing)
Features: Lacrimal fossa (for lacrimal
gland)
Optic foramen
Trochlear fossa
Lateral wall: Sphenoid (anterior surface of
the greater wing)
Zygomatic (orbital surface)
Features: Zygomatic canal (for zygomatic
nerve from maxillary nerve)
Floor (Inferior) wall: Maxilla (orbital
surface)
Zygomatic bone
Palatine bone (orbital process)
Features: Infra orbital groove and canal
*Superior Orbital Fissure: separates the
lateral wall from the roof.
*Inferior Orbital Fissure: separates the
floor from the lateral wall.
Pterygopalatine
Fossa
Roof: Inferior surface of body of sphenoid
Orbitalprocess of palatine bone
Inferior orbital fissure
Floor: Apposition of anterior and posterior
walls of the fossa
Anterior wall: Upper part of posterior
surface of maxilla
Posterior wall: Anterior surface of greater
wing of sphenoid
Root of pterygoid process
Anterior opening of pterygoid canal
Medial wall: Upper part of perpendicular
plate of palatine bone
Orbital and sphenoidal processes of palatine
bone
Sphenopalatine foramen
Mandible
- Body: Surfaces ( external and internal )
Borders ( upper and lower )
Mental protuberance
Mental tubercle
Mental foramen
Oblique line
Digastric fossa
Mylohyoid line
Submandibular fossa
Sublingual fossa
Mental spines
Mylohyoid groove
2. Ramus: Surfaces ( lateral and medial )
Borders ( anterior and posterior )
Mandibular notch
Coronoid process
Condylar process ( head and neck of the
mandible )
Angle of the mandible
Mandibular canal
Lingula
|
Foramina
of Middle Cranial Fossa |
|
Optic Canal |
|
|
Superior Orbital Fissure |
|
|
Foramen Rotundum |
|
|
Foramen Ovale |
|
|
Foramen Spinosum |
|
|
Foramen Lacerum |
|
|
* all
structures pass through sphenoid bone |
|
Foramina
of Posterior Cranial Fossa |
|
Internal auditory meatus |
|
|
Jugular foramen |
|
|
Hypoglossal canal |
|
|
Foramen magnum |
|
|
* all
structures pass through temporal & occipital bone |
|
Passage
of Cranial Nerves |
|
CN I |
|
|
CN II |
|
|
CN III, IV, V1, VI |
|
|
CN V2 |
|
|
CN V3 |
|
|
CN VII, VIII |
|
|
CN IX, X, XI |
|
|
Mastication
muscles |
|
|
3
Structures in Carotid sheath |
|
|
Diaphragm |
||
|
Embryology |
|
|
|
Passage |
At T 8 |
Inferior vena cava |
|
At T10 |
esophagus, vagus |
|
|
At T12 |
aorta, thoracic duct, azygous vein |
|
|
Innervation |
C3,4,5 : Referred pain to shoulder |
|
|
8
Layers of Abdomianl wall |
Spermatic
cord |
|
Skin |
|
|
Fascia ( Camper's & Scarpa's
) |
Dartos muscle & Colles'
fascia |
|
Ext. Oblique muscles |
Ext. spermatic fascia &
superficial inguinal ring |
|
Int. Oblique muscles |
Cremaster muscle & conjoint
tendon |
|
Transeverse abdominalis |
No contribution except to
conjoint tendon |
|
Transverse facisa |
Internal spermatic fascia &
deep inguinal ring |
|
Extraperitoneal fat |
|
|
Peritoneum |
Tunica vaginalis testis &
processus vaginalis |
|
Inguinal
Hernia |
|
|
Direct
Hernia |
|
|
Indirect
Hernia |
|
|
Hasselbach's
triangle |
|
|
Clinical
Landmarks |
|
|
Ischial
spine |
|
|
McBurney's point |
|
|
Iliac crest
|
|
|
Hand
Muscle : Thenar - Hypothenar |
|
|
Thenar
|
|
|
Hypothenar |
|
|
Contents
of femoral sheath |
|
lateral
to medial |
|
femoral
nerve, artery, vein, lymphatics |
|
femoral
nerve lies outside femoral sheath |
|
femoral
canal contains deep inguinal lymph node |
|
Unhappy
triad of Knee injury |
|
|
Anterior Drawer sign :
indicate tearing of ant. crucate ligament |
|
Muscle
name with Palate |
|
|
KLM
sounds |
||
|
Kuh- kuh-kuh |
test palatal elevation |
vagus nerve |
|
La- la- la |
test tongue |
hypoglossal nerve |
|
Mi- mi- mi |
test lips |
facial nerve |
|
Muscle
name with ~Glossus |
|
|
Cervical
rib |
|
|
|
Medial
nerve injury |
|
|
Motor
deficit |
|
|
Sensory
deficit |
|
|
Ulnar
nerve injury |
|
|
Motor
deficit |
|
|
Radial
nerve injury |
|
|
Motor
deficit |
|
|
Sensory
deficit |
|
|
Axillary
nerve injury |
|
|
Motor
deficit |
loss of
deltoid action |
|
Musculocutaneous
nerve injury |
|
|
Motor
deficit
|
loss of function of
coracobrachialis, biceps & brachialis muscle ( biceps reflex )
|
|
Sensory
deficit |
|
|
Erb-
Duchenne palsy |
|
|
Cause |
Traction or tear of the superior trunk of
the brachial plexus (C5 & C6 roots) |
|
Findings |
|
|
Nerve
injury in lower limbs |
|
|
|
|
|
|
|
|
|
|
Pectinate
line |
|
|
|
|
|
|
Portal
- systemic anastomosis |
|
|
|
|
|
|
|
|
Recurrent
laryngeal nerve |
|
|
|
|
wraps around the aortic
arch and the ligamentum arteriosum |
|
wraps around right
subclavian artery. |
|
|
|
Lung
relations |
|
|
|
|
Course
of ureter
|
|
|
Autonomic
innervation of penis |
|
|
|
|
|
|
|
|
Ligaments
of the uterus |
|
_____________________________________________________________________________________
- skeleton of head most complex bony structure in body, it encloses
brain, houses organs of special senses, and surrounds openings into
respiratory and digestive tracts
- in anatomical position, skull orientated so that inf margin of
orbit and sup margin of external auditory meatus are level (orbitomeatal plane, Frankfort plane)
Anterior Aspect
- comprises ant part of calvaria superiorly and
skeleton of face inferiorly
- notable features are forehead, orbits, prominence
of cheek, anterior nasal apertures, paired maxillae, and mandible
- can be divided into five areas: frontal,
orbital, maxillary, nasal and mandibular
Posterior
Aspect
- formed mainly by paired parietal bones and
occipital bone, meet mastoid parts of temporal bones laterally
- most prominent feature is
rounded post pole, occiput, this region often referred
to as occipital area
- external occipital protuberance is median projection, easily palpable at sup
end of med furrow of neck
- centre and most prominent projection
called inion
- curved superior nuchal
lines run lat from ext occipital protuberance towards mastoid
processes, represent sup limit of post neck, indicated where certain neck
muscles attach
- post part of sagittal suture and lambdoid
sutures meet at lambda
Superior Aspect
- oval shaped, broadened post by
parietal eminences
- superciliary arches of frontal bone from ant limit, zygomatic
arches visible laterally
- four bones united by interlocking sutures
- two parietal bones joined by sagittal suture
- frontal and parietal bones joined by coronal suture
- parietal and occipital bones
joined by lambdoid sutures
- intersection of coronal and
sagittal sutures is called bregma
- vertex, most sup part of skull, located near centre of
sagittal suture
- parietal foramina located in parietal bone on each side of
sagittal suture, transmit emissary veins which connect intracranial dural
sinuses with veins covering skull
Inferior Aspect
- external surface of cranial base shows maxilla,
bony palate, maxillary teeth and zygomatic arches
- each zygomatic arch formed by union of
zygomatic bone and zygomatic process of temporal bone
- centrally, inf surface of cranial base
irregular due to many foramina, processes and articulations, makes it
weak and prone to fractures
- lat, cranial base exhibits
temporal bones with prominent mastoid and styloid processes
- foramen magnum, bordered lat by occipital
condyles (articulate with C1), transmits medulla oblongata
Lateral Aspect
- includes parietal, frontal and parts of
temporal and sphenoid bones
- division of skull into calvaria and facial
skeleton clearly shown
- calvaria formed by frontal bone (ant), sphenoid
and parietal bones (lat), and occipital bone (post)
- pterion (where all four bone articulate) is important clinical
landmark (ant branch of mid meningeal a. lies beside), located in temporal fossa
- located 2 fingers sup to zygomatic arch, 1
thumb post to zygomatic process of frontal bone
- other features are external auditory meatus,
zygomatic bone, zygomatic arch, mastoid process and mandible
- mastoid process project ant-inf, med to ear
lobe, easily palpable, size varies with muscularity and age (not present
at birth, enlarge at puberty), form part of sup attachment of
sternocleidomastoid
- mental protuberance (of chin) easily visible in
most people
Internal Aspect
- bones seen in internal aspect of skull are:
frontal, ethmoid, sphenoid, temporal and occipital
- internal surface of calvaria fairly smooth and
concave, particularly from side to side
- striking features are grooves in parietal bones
made by ant branches of mid meningeal blood vessels
- sutures least distinct on
inside because fusion begins ~10 years earlier
- arachnoid granulations project into venous sinuses (particularly into
lacunae of sup sagittal sinus) enough to indent bones of calvaria
- presents three distinct tiered
areas: anterior, middle, and posterior
cranial fossae
Walls
- thinner in females, young and old
- tends to be thinnest in areas that are well
covered by muscles
- most bones of calvaria consist of inner and
outer layers (tables) of compact bone, separated by layer of spongy diploë (containing red bone marrow)
Bones of Calvaria
- except for mandible and auditory ossicles bones of skull are joined
by rigid sutures
- cranium is essentially one big complex bone
Frontal Bone
- frontal squama = smooth, board, convex plate of bone forming
forehead
- the two halves halves of frontal squama are
divided by metopic (frontal) suture in
foetal skulls, begins to fuse during infancy and is not usually visible
after 6 years of age
- frontal bone forms thin roof of orbits
- just sup to and parallel to each supraorbital
margin is bony ridge called superciliary arch,
which overlies frontal sinus
- gently rounded glabella
lies between the two arches
- slightly prominences on each
side (sup to superciliary arches) are frontal eminences
- supraorbital notch (foramen) (transmits supraorbital vessels and nerve)
located in med supraorbital margin
- articulates with nasal bone at
frontonasal suture
- at point where this crosses internasal suture is an anthropological landmark,
nasion
- this isdepression in root of nose, where it
joins cranium
- also articulates with zygomatic, lacrimal,
ethmoid and sphenoid bones
Parietal bones
- form large parts of wall of calvaria
- face extends from margin of hair to chin, from one auricle to or
- forehead common to both face and scalp
- skin contains numerous sweat and sebaceous glands and is connected
to underlying bones by loose ct
- superficial fascia lies beneath skin with muscles of facial
expression are embedded in it
Sensory Nerves
- include branches from three division of trigeminal n., which supply
skin of face (except for small area over angle of mandible and parotid
gland supplied by greater auricular n.,
C2-3)
Ophthalmic
Nerve (V1)
- superior division of trigeminal nerve
- wholly sensory and supplies skin derived from frontonasal prominence
- divides into three branches
just before entering sup orbital fissure: nasociliary, frontal and lacrimal
Nasociliary
- supplies tip of nose through external nasal
branch of anterior ethmoidal n.
- supplies root of nose through infratrochlear n.
Frontal
- direct continuation of V1
- divides into two branches: supraorbital (med) and supratrochlear (lat)
Lacrimal
- smallest of main ophthalmic branches
- emerges over sup-lat orbital margin to supply
the lat part of upper eyelid
Maxillary Nerve
(V2)
- intermediate division of trigeminal nerve
- three cutaneous branches
supply skin derived from maxillary prominence
- infraorbital n. (large terminal branch) passes through
infraorbital foramen and supply skin on lat nose, upper lip and lower
eyelid
- zygomaticofacial n. (small branch) emerges from
zygomatic bone through zygomaticofacial foramen to supply skin over
zygomatic prominence
- zygomaticotemporal n. emerges through zygomaticotemporal foramen and
supplies skin over temporal region
Mandibular
Nerve (V3)
- inferior division of trigeminal nerve
- three sensory branches supply
skin derived from mandibular
prominence, and
motor fibres supply muscles of mastication (only division to carry motor
fibres)
- buccal n. emerges deep to ramus of mandible to supply skin of
cheek over buccinator, mucous membrane lining and post part of gingival
surface
- auriculotemporal n. passes med to neck of mandible
and n turns up, post to it head and ant to auricle, n crosses over root
of zygomatic process, deep to superf temporal a., supplies parts of auricle, ext acoustic meatus,
tmpanic mebrance and skin in temporal region
- inf alveolar n. (large terminal branch) enters mandibular canal
through mandibular foramen, supplies branches to lower teeth, opposite
mental foramen divides into incisive (incisor teeth) and mental (chin) branches
- lingual n. (small terminal branch) supplies general
sensory fibres to ant 2/3 of tongue, floor o f mouth and mandibular gums
Motor Nerves
- CN VII (facial n.) supplies platysma, muscles of facial expression,
auricular and scalp muscles
- sole motor supply to muscles of facial expression, taste sensation
from ant 2/3 of tongue, and secretomotor to salivary glands
(except for parotid)
- emerges from skull through
stylomastoid foramen (between mastoid and styloid processes), almost
immediately enters parotid gland, runs superficially, gives off five
terminal branches: temporal, zygomatic, buccal, mandibular
and cervical
- emerge from sup, ant and inf margins of parotid gland and spread
out like abducted digits
Arterial Supply
- two main arteries supply most
of blood to face: facial and superior temporal aa.
- branches from supraorbital and supratrochlear supply skin of
forehead
Facial Artery
- chief a. of face
- arises from ext carotid and winds it was to inf
mandible just ant to masseter, usually grooving bone, lies superf here
and pulsations can easily be felt
- crosses mandible, buccinator and maxilla, lies
deep to zygomaticus major and levator labii superioris
- branches on face include submental, inferior
labial, superior labial, and lat nasal
Superficial
Temporal Artery
- smaller of two terminal branches of ext carotid
a.
- begins within parotid gland,
post to neck of mandible, ascends superf to post part of zygomatic
process, enters temporal fossa and ends in scalp by dividing into frontal
and parietal branches
- transverse facial a. arises from superf temporal a. before it
emerges from parotid gland, crosses face superf to masseter, about
fingerbreadth inf to zygomatic arch , supplies parotid gland, masseter
and skin of face, anastomoses with branches of facial a.
Venous Drainage
- facial vein is major route of drainage from face
- formed by union of supraorbital and
supratrochlear vv. at med angle of eye
- connected sup ophthalmic v. through supraorbital v. (near zygomatic process)
- connected to cavernous sinus by ophthalmic v.
- crosses superf to
submandibular gland and is joined by anterior division of retromandibular v. to form common facial v., which ends by draining into internal jugular v.
Retromandibular
Vein
- formed by union of superf
temporal and maxillary vv., post
to neck of mandible
- descends within parotid gland, superf to ext carotid a. but deep to facial n.
- divides into ant branch that
unites with facial v. and post branch that joins posterior auricular v. to form external jugular v.
Lymph Drainage
- forehead and ant face submandibular nodes
- lat face parotid nodes
- central lower lip and chin submental nodes
Muscles of Face
- embedded in superficial fascia
- most arise from bones of face and insert into skin, they don’t move
bony structures
- orbit, nose and mouth are guarded by eyelids, nostrils and lips
respectively
- facial muscles serve as sphincter, or dilators
of the facial openings
- all develop from 2nd pharyngeal arch and are supplied by
facial n. (VII cranial)
|
Notes |
|
|
|
||
|
Eye |
orbicularis oculi |
sphincter (narrows eye and encourages
secretion of tears) |
three parts: orbital (closing eyes
tightly), palpebral (closing eyes lightly), lacrimal (pulls eye med) |
||
|
Nose |
nasalis |
compression/dilation of nostril |
compressor naris: rudimentary in human dilators of nose: flare the alar
cartilages of nose |
||
|
Mouth |
orbicularis oris |
sphincter |
fibres derived from buccinator and or
facial muscles |
||
|
dilator muscles |
|
radiate out like spokes |
|||
|
buccinator |
presses cheeks against teeth |
attached to alveolar processes and
pterygomandibular raphe fibres mingle with orbicularis oris |
|||
- covers vault of skull and extends sideways between right and left
temporal lines, between eyebrows anteriorly and sup nuchal lines
posteriorly
|
|
|
Scalp |
|
Boundaries |
|
covers vault of skull lat: temporal lines ant: eyebrows post: sup nuchal line |
|
Contents |
Arteries |
from int carotid (supraorbital,
supratrochlear) from ext carotid (superf temporal, post
auricular occipital) |
|
Veins |
supratrochlear & supraorbital (
facial) superf temporal + maxillary (
retromandibular) post auricular + post retromandibular (
ext jugular) occipital ( suboccipital plexus
vertebral) emissary (communication with inside of
skull) |
|
|
Nerves |
trigeminal (supratrocheal, supraorbital,
zygomatico-temporal, auriculo-temporal) C2 (greater & lesser occipital) |
|
|
Muscles |
occipitofrontalis tempoparietalis |
|
|
lymph |
scalp above parotid gland parotid
lymph nodes scalp above auricle
retroauricular lymph nodes back of scalp occipital lymph
nodes |
|
|
Notes |
|
trigeminal supply ant to line between ears
and vertex, C2 supplies rest |
Layers
- has five layers, of which first
three are intimately bound toger: skin, connective tissue, aponeurosis epicranialis (scalp proper), loose
areolar tissue,
and pericranium
- mobile because of potential cleavage plane
Epicranial
Aponeurosis
- strong membranous sheet that covers sup aspect
of calvaria
- aponeurosis is membranous tendon of fleshly
bellies of epicranial muscle (formed by occipitalis and frontalis
muscles, each with two bellies: 2 frontal & 2 occipital)
- muscles are supplied by facial nerve (VII)
Applied Anatomy
- scalp richly supplied by blood small
lacerations may bleed profusely
- tension of epicranial aponeurosis (produced by
occipitofrontalis) means that deep wounds dividing aponeurosis will gape
- infection of scalp may occasionally spread (via
emissary vv.) to skull bones, infected
blood in diploic vv. may travel via
emissary vv. into venous sinuses and produced venous sinus thrombosis
- cranial base has three levels
called anterior, middle and posterior cranial fossae
- each fossa slightly inferior to one rostral to it
Anterior Cranial Fossa
- occupied by of frontal lobes of cerebral hemispheres
- formed mainly by frontal bone (ant boundary)
- most floor composed of convex orbital parts (bone roof of orbits)
- shows sinuous, shallow depression called
convolution impressions or brain markings,
possibly formed by the gyri of the brain
- crista galli is
median process (resembling cock’s crest) that projects sup from ethmoid
bone
- on both sides of crista galli is a narrow, cribriform
plate, with numerous foramina for olfactory nn.
- lesser wings and jugum of sphenoid bone form posterior floor
(boundary) of fossa
- lesser wings have sharp post spenoidal ridges that overhang ant middle fossa
and project into ant part of lateral sulci
- each lesser wing ends med in ant clinoid process which gives attachment to
tentorium cerebelli
Middle Cranial Fossa
- occupied by temporal poles and ~˝ of inf surface of temporal lobe
- marked off from posterior fossa by dorsum
sellae (med) and sup border of petrous part of temporal bone (lat),
and from ant fossa by posterior edge of lesser wing of sphenoid
- saddle-like part of spenoid bone (between ant & post clinoid
processes) known as sella turcica, composed
of three parts:
- tuberculum sellae: ant, olive-shaped swelling
- hypophoseal fossa: mid, seat-like depression
- dorsum sellae: post, median rectangular
projection
Posterior Cranial Fossa
- largest and deepest of fossae
- occupied by pons, cerebellum and medulla
- formed largely by inf and ant occipital bone, but sphenoid and
temporal bones also contribute
- broad bony grooves formed by transverse
sinuses lie between diverging folds of tentorium cerebelli (groove
for right usually larger because sup sagittal sinus usually enter on
right)
- foramen magnum
located in centre of fossa
- rostral to foramen, basilar
part of occipital bone rises to meet sphenoid bone, called clivus
- internal occipital crests is bony crest that lies post and sup to foramen magnum
- partly divides post cranial fossa into two cerebellar fossae that lodge cerebellar
hemispheres
- end sup and post inirregular
elevation called internal
occipital protuberance
- vermis of cerebellum lies in vermian fossa, just post to foramen magnum
Foramen
Ovale
- Mandibular div. of trigeminal
- Accessory meningeal A.
- Lesser petrosal N.
Foramen
spinosum
- Middle meningeal A.
- Meningeal branch of mandibular
N.
Carotid
canal
Int.
carotid A. with venous and sympathetic plexuses
Palatovaginal
canal
- Pharyngeal branch of
pterygopalatine ganglion
- Minute pharyngeal branch from 3rd
part of maxillary artery
Pterygoid
canal
Nerve of
pterygoid canal
Sphenoidal
emissary foramen
Emissary
vein from cavernous sinus
Foramen
lacerum
- Int. carotid A.
- Deep petrosal N.
- Greater petrosal N.
- Meningeal branches of ascending
pharyngeal A.
- Emissary vein from cavernous
sinus.
2 and 3
join to form N. of pterygoid canal.
Foramen
magnum
- Apical ligament of dens
- Membrana tectoris
- Medulla oblongata
- Meninges
- Spinal roots of accessory N.
- Vertebral A. with sympathetic
plexus
- Post. spinal A.
- Ant. spinal A.
Hypoglossal
canal
- Hypoglossal N
- Meningeal br. of ascending
pharyngeal A.
- Emissary vein from basilar
plexus
Jugular
foramen
- Inf. petrosal sinus
- Glossopharyngeal N.
- Vagus N.
- Accessory N.
- Int. jugular V.
- Sigmoid sinus
Condylar
canal
Emissary
vein from sigmoid sinus
Stylomastoid
foramen
- Facial N.
- Stylomastoid br. of post.
auricular A.
Cribriform
plate of ethmoid
Olfactory
N form nasal mucosa to olfactory bulb
Ant.
ethmoidal canal
- Ant. ethmoidal N.
- Ant. ethmoidal vessels
Post.
ethmoidal canal
Post.
etmoidal vessels
Optic
canal
- Optic N.
- Ophthalmic A.
- Meninges
Superior
orbital fissure
- Terminal branches of ophthalmic
N.
- Ophthalmic V.
- Occulomotor
- Trochlear
- Abducent
Foramen
rotundum
Maxillary
N.
Internal
acoustic meatus
- Facial N.
- Vestibulocochlear N.
- Nervus intermedius
- Labyrinthine vessels
Facial
canal
Facial
N.
Mastoid
foramen
- Emissary V. from transverse
sinus
- Meningeal branch of occipital A.
Foramina of the skull
|
|
Foramina |
Contents |
|
|
|
Or |
Nerves |
|
|
Anterior |
foramen cecum |
nasal emissary v. (present in children and
1% of adults) |
|
|
foramina in cribiform plates |
|
axons of olfactory cells |
|
|
ant & post ethmoidal foramina |
vessels and nn. with same names |
|
|
|
Middle |
optic canals |
ophthalmic aa. |
CN II |
|
sup orbital fissures* |
ophthalmic vv. |
CN V1, III, IV, VI, SNS |
|
|
foramen rotundum* |
|
CV V2 (maxillary n.) |
|
|
foramen ovale* |
accessory meningeal a. |
CN V3 (mandibular n.) |
|
|
foramen spinosum* |
mid meningeal vessels |
meningeal branch of CN V3 |
|
|
foramen lacerum* |
int carotid a. accompanying sympathetic and venous
plexuses |
|
|
|
hiatus of greater petrosal n. |
petrosal branch of mid meningeal a |
greater petrosal n. |
|
|
Posterior |
foramen magnum |
vertebral, ant & post spinal aa. dural vv. |
medulla and meninges spinal roots of CN XI |
|
jugular foramen |
sup bulb of int jugular v., inf petrosal
& sigmoid sinuses meningeal branches of asc pharyngeal and
occipital aa. |
CN IX, X, XI |
|
|
hypoglossal canal |
|
CN XII |
|
|
condylar canal |
emissary v. |
|
|
|
mastoid foramen |
mastoid emissary v. meningeal branch of occipital a. |
|
|
- *
part of crescent of foramina
- brain is enveloped by three
membranes: dura mater, arachnoid mater and pia
mater (arachnoid +
pia = leptomeninges), collectively known as cranial meninges
- continuous with spinal meninges covering spinal cord
- cranial meninges and CSF provide support and protection for brain
Dura Mater
- outermost and toughest of cranial meninges
- consists of collagenous connective tissue
- dura mater loosely attached to calvaria, but tightly attached to
base
- fractures of base more easily damage dura
leading to leakage of CSF out of nose and ear
- two layered structure
- inner: meningeal
- outer: endosteal
- internal layer continuous with spinal dura at foramen magnum
- provides tubular sheaths for CNS as they pass through foramina in
floors of cranial fossae; outside skull theyy fuse with epineurium, dural sheaths of cranial nerves extend
approximately to cranial ganglia
- trigeminal ganglion surround by extension of
cranial meninges, occupies trigeminal cave in
trigeminal impression in petrous part of temporal bone
- dural sheath of optic nerve continuous with int
meningeal layer of cranial dura and sclera of eye
Dural Septa or
Reflections
- during development of brain, dura duplicated to
form four inwardly projecting dural septa
- septa divide cranial cavity into three
intercommunicating compartments, one subtentorial and two supratentorial
Falx Cerebri
- large, sickle shaped vertical partition in
longitudinal fissure between hemispheres
- attached in median place to int surface of
calvaria from frontal crest of frontal bone and crista galli
of ethmoid bone ant, and int occipital protuberance post
- also attached to midline of tentorium
cerebelli
- at sup border, its two layers separate to
enclose sup sagittal sinus, free
inf edge encloses inf sagittal sinus
- forms rigid partition between hemispheres and
reduces side-to-side movement
Tentorium
Cerebelli
- wide tent-shaped, arched fold of dura
- separates occipital lobes from cerebellum
- med attachment of falx cerebri holds tentorium
cerebelli up
- attached ant-lat to sup petromastoid
parts of temporal bones and ant & post clinoid processes
- attached post to occipital bone along grooves
for transverse sinuses, which it encloses
- U-shaped ant border is free, between it and
dorsum sellae is opening called tentorial notch,
which surrounds midbrain
Falx Cerebelli
- small, sickle-shaped median dural fold in post
post cranial fossa
- extends almost vertically, inf to inf tentorium
cerebelli
- free-edge projected slightly between cerebellar
hemispheres
- occipital sinuses contained in fixed edge
Diaphragma
Sellae
- small, circular, horizontal sheet of dura
formsroof for hypophyseal fossa
- formed by dura surrounding pituitary gland and
encircling its stalk
Arteries
- many meningeal aa. in periosteum supply most
blood to periosteum, not meninges!
- only very fine branches of are
distributed to dura
- middle meningeal a. is largest of meningeal aa., branch of
maxillary a., embedded in dura, clinically imp because it can be torn
when skull is fractured
- enters cranial cavity through
foramen spinosum, runs lat along floor of the middle cranial fossa,
turns sup-ant on greater wing of sphenoid, where it divides into ant and
post branches
- ant branch runs sup to pterion and curves post to ascend
towards vertex of skull, often found inbony tunnel in region of pterion
- post branch runs post in groove in squamous part of
temporal bone, n ramifies all over post skull
- all meningeal aa. accompanied by veins, lie
between aa. and bones
Nerve Supply
- rich sensory supply largely through three
divisions of trigeminal n.
Arachnoid Mater
- delicate, transparent membrane, composed of weblike tissue
- forms intermediate covering of
brain and separated from dura by film of fluid in potential subdural space
- it does not closely investment of brain, but passes over sulci and
fissures
- separated from pia by subarachnoid space
- numerous trabeculae pass from arachnoid to pia, givingweblike
structure
Pia Mater
- very thin, highly vascularised, loose connective issue membrane
that adheres closely to surface of brain
- dips into all sulci and fissures and carries blood vessels with it
- cerebral veins run on pia within subarachnoid space
- when branches of cerebral vessels penetrate brain, pia follows for
a short distance, forming sleeve of pia, refore perivascular
spaces are continuous with subarachnoid space
Venous Sinuses of Dura Mater
- sinuses are venous channels located between dura and int endosteal
lining of cranium
- drain all blood from brain
Superior
Sagittal Sinus
- lies in superior border of falx cerebri
- usually ends by becoming right transverse
sinus
- dilation at termination known as confluence of sinuses as five sinuses
communicate with it
Inferior
Sagittal Sinus
- lies in inf border of falx cerebri
- much smaller than sup sagittal sinus
- ends by joining great cerebral v. to form
straight sinus
Straight Sinus
- runs along the line of attachment of falx
cerebri to tentorium cerebelli
- ends by joining one of transverse sinuses,
usually left
Transverse
Sinus
- pass lat from confluence of sinuses in attached
border of tentorium cerebelli
- leave tentorium and become sigmoid sinuses
Sigmoid Sinuses
- follow S-shaped course in post cranial fossa,
forming deep groove in the temporal and occipital bones, turn ant and
enter sup bulbs of int jugular vv.
Occipital Sinus
- lies in attached edge of falx cerebelli
Superior and
iferior Petrosal Sinuses
- they drain the cavernous sinus into the
transversesinus and int j v respectively
Cavernous Sinuses
- large venous sinuses, 2 cm x 1 cm, capacity:
1.5 ml
- located on eir side of pituitary in sella
turcica
- runs from apex of orbit to apex of petrous
temporal bone
- contain many blood channels formed by numerous
trabeculae
Receives blood
from:
- sup and inf ophthalmic vv. (orbit)
- superf mid cerebral v. (brain)
- sphenoparietal sinus (skull)
- intercavernous sinuses (cavernous sinus of or
side)
Drains blood
into
- sup and inf petrosal sinuses
- pterygoid venous plexus
Relations
- ant: apex of orbit
- post: brain stem (junction of peduncle with
pons)
- med: body of sphenoid bone and pituitary fossa
- lat: temporal lobe
- sup: int carotid a., uncus of temporal lobe
- inf: greater wing of sphenoid
Immediate
relations
- lat: oculomotor, trochlear, ophthalmic, and
maxillary nn.
- inside sinus but outside blood: int carotid a.,
abducens n.
- oral cavity is
divided into vestibule and mouth proper
- vestibule lies within cheek and lips, but outside gums and teeth
- mouth cavity communicates post with pharynx through oropharyngeal isthmus
(isthmus of fauces)
- bounded by soft palate above, tongue below and
palatoglossal arches on each side
- palate (hard and soft) forms roof of mouth
Lips
- covered ext by skin, int by mucous membrane
- contains part of orbicularis oris
- attach to gum by frenulum
- mucous labial glands moisten lip
- meet at angles (labial commisures) of mouth
Cheeks
- directly continuous with lips and have same
general structure
- buccinator forms muscle layer
General Features
- three parts: root (or base, post 1/3, post-sulcal,
pharyngeal part); body (or ant 2/3, pre-sulcal, oral
part); and tip
- two surfaces: upper (dorsum) and lower (ventrum)
- upper surface divided into two parts by V shaped sulcus terminalis: ant
2/3 oral part, post 1/3 pharyngeal part
- foramen caecum located at apex of V
- mucous membrane of the upper surface of the
oral part is rough due to presence of numerous lingual papillae
- mucous membrane of the lower surface of the
oral part is smooth , devoid of papillae, and shows visible deep lingual
v. either side of frenulum
- post 1/3 is devoid of papillae but
has a nodular irregular surface caused by the underlying lymph nodules
called lingual tonsil.
- the interval between the post 1/3of the tongue and the
epiglottis is part of oropharynx and shows: median and lateral
glossoeppiglottic folds, and vallecullae (a small depression detween the
two folds)
Lingual
Musculature
|
Muscles |
Main
actio |
Nerve
supply |
|
|
Extrinsic |
genioglossus |
protrusion |
CN XII |
|
hyoglossus |
depression |
||
|
styloglossus |
retraction |
||
|
palatoglossus |
elevation |
Pharyngeal plexus |
|
|
Intrinsic |
sup longitudinal muscle |
they change the shape of the tongue |
CN XII |
|
inf longitudinal muscle |
|||
|
transverse muscle |
|||
|
vertical muscle |
|||
Nerve Supply
|
|
|
Ant
2/3 |
Post1/3 |
|
Sensory |
General |
lingual (CN V) |
glossopharyngeal |
|
Special |
chorda tympani (CN VII) |
||
|
Motor |
hypoglossal (except for palatoglossus,
supplied by CN X) |
||
Arterial Supply
- major: lingual a.
- also tonsillar and asc palatine branches of
facial a.
Venous Drainage
- all veins on one side unite to
form lingual v., which drains into int jugular or facial
v.
Lymphatics
- tip: submental
- ant 2/3: submandibular (central cross to
opposite side as well)
- post 1/3: deep cervical
Applied Anatomy
- glossitis usually accompanies stomatitis
- in acute glossitis, oedema and swelling of
tongue are marked (facilitated by loose c.t. and plenty of lymphatics)
- in some anaemias and vitamin deficiencies
tongue becomes bald, due to atrophy of filiform papillae
- lesion of hypoglossal n. results in paralysis
of affected side and hemiatrophy, when patient tries to stick out tongue,
deviates to paralysed side
- in unconscious patient, post tongue may fall
back and cause laryngeal obstruction
- carcinoma of post tongue has poor prognosis due
to bilateral lymphatic spread
Hard Palate
- skeleton: palatine process of maxilla, horizontal plate of palatine
- alveolar margin: teeth and gums
- post margin: soft palate
- oral surface: stratified squamous keratinised epith, mucosa adheres
to bone, palatine raphe, transverse palatine folds, mucosal glands
prominent
Soft Palate
- base: attached to post hard palate
- free post border presents uvula in midline
- palatoglossal folds extend
inf and ant; and palatopharyngeal folds extend
inf and post from the under surface of the soft palate
- has oral (lower) and pharyngeal (upper) surfaces
Structure
- oral mucosa on oral surface and adjoining
pharyngeal surface; rest covered by respiratory mucosa
- core is palatine aponeurosis with levator
palati on upper surface and palatopharyngeus and palatoglossus on lower surface
Muscles
- tensor and levator palati
- musculus uvulae
- palatoglossus
- palatopharyngeus
Blood Supply
- branches of maxillary a. (greater and lesser
palatine aa.)
- veins drain into pterygoid venous plexus
Lymphatics
- drain into submandibular, retropharyngeal, and
deep cervical nodes
Nerve Supply
- sensory: greater and lesser palatine nn.,
nasopalatine n.
- motor: pharyngeal plexus, except tensor palati
supplied by mandibular n.
- lies between body of mandible and hyoid bone
- superficial part includes submental and
digastric triangles
- deeper parts include root of tongue and floor
of mouth
Structures
- muscles: digastric, stylohyoid, mylohyoid, hyoglossus
- submandibular gland
- mixture of serous and mucous acini
- two parts: superficial and deep
- superficial: in digastric triangle, reaching
upward under cover of mandible, separated post from parotid gland by
stylomandibular lig
- deep: extends forwards in interval between
mylohyoid and hyoglossus, post end continuous with superf part of gland,
while ant end reaches as far as sublingual gland
- coverings: inner ct capsule and outer fibrous
capsule (derived from deep cervical fascia)
- submandibular duct: runs from ant deep
submandibular gland, forward between mylohyoid and hyglossus
- blood supply: branches of lingual and facial,
veins follow aa.
- nerve supply: derived from submandibular
ganglion (receives parasympathetic fibres from chorda tympani, lingual
and sympathetic trunk)
- applied submandibular salivary gland
- common site of calculus formation
- presence of tense swelling below body of
mandible, greatest before and during meal and reduced in size or absent
between meals
- largest of salivary glands (branched serous acini)
- very irregular shape because it’s wedged in among number of structures
- covered by a capsule and a dense fibrous tissue sheath (parotid fascia) formed
by deep cervical fascia
- divided into two (superficial and deep) parts by facial n.:
Position and
Extent
- lies in fossa post to ramus of mandible
- extends from external acoustic meatus to upper
part of carotid triangle
- med, extends to styloid process and around neck
of mandible
- post, overlaps sternocleidomastoid and extends
ant over masseter
- portion of facial part often detached and
called accessory parotid gland
- wedge-shaped (base above, apex behind angle of
mandible)
- sup: extends upward behind TM joint into post
mandibular fossa, called glenoid process
- ant: extends forwards superf
to masseter, called facial process
Parotid Duct
- 5 cm long, 5mm wide
- passes horizontally from ant edge, turns med at
ant masseter and pierces buccinator, and enters oral cavity opposite
crown of 2nd maxillary molar tooth
Structures
within the Gland
- facial n (superf)
- retromandibular v
- external carotid a. (deep)
Nerve and blood
Supply
- supplied by branches of external carotid a., drains by tributaries of retromandibular v.
- secretomotor (parasympathetic): from glossopharyngeal n. (IX), via otic ganglion
- sensory: branches from greater auricular and
auriculo-temporal nn.
Applied Anatomy
- sup part of respiratory tract and contains peripheral organ of
smell
- divided into right and left
nasal cavities by nasal septum
- its mucosa is divisible into olfactory and respiratory areas
- functions include
- respiration
- olfaction
- filtration of dust
- humidification of inspired
- receives secretion form paranasal sinuses and
nasolacrimal ducts
Skeleton of External Nose
- immovable bridge of nose (sup bony part of nose) consists of nasal bones,
frontal processes of maxillae and nasal part of frontal bone
Nasal Septum
- bony part of septum usually located in med
plane, until 7 years of age when it deviates slightly to one side (more
frequently right)
- nasal septum has three main components
- perpendicular plate of ethmoid bone: (forms sup
part, very thin, desc from cribriform plate)
- vomer: (forms post-inf part, thin, flat bone)
- septal cartilage
- movable cartilaginous
part of nose consits of five main cartilages andfew smaller ones
- composed of hyaline cartilage
- connected with one anor and nasal bones by
continuity of perichondrium and periosteum
- U-shaped alar nasal
cartilages are free and movable, can dilate and constrict nares
Nasal Cavities
- nasal cavity opens anteriorly
through nostrils or ant nares
- open posteriorly into nasopharynx through choanae
(post nasal aperture)
- mucosa lines entire nasal cavity, except vestibule
- entrance to vestibule of nose
is lined with skin containing hairs called vibrissae
- nasal mucosa is
tightly bound to periosteum and perichondrium of supporting structures
- continuous with lining of all chambers with
which nasal cavities communicate
- inf 2/3 called respiratory area, and sup 1/3 called olfactory area
Walls
- floor: palatine process of maxilla, horizontal plate of palatine bone
- roof:
nasal bone, frontal bone, cribriform plate of ethmoidal bone and body of
sphenoidal bone, communication with cranial cavity through cribriform
plate
- septum: formed by vomer, perpendicular plate of ethmoid, septal
cartilage, fibrofatty tissue of mobile septum
- lateral wall: skeletal framework : nasal bone; frontal process of maxilla,
lacrimal,; ethmoid labyrinth with sup and mid conchae, inf concha,
perpendicular plate of palatine bone, med pterygoid plate
- uneven due to three shelf-like projections
called superior, middle and inferior conchae
- sphenoethmoidal recess lies above sup concha;
other spaces are sup, middle and inf meatuses lie below the corresponding
conchae
- hiatus semilunaris is a curved cleft (window)
in the middle meatus, lies between bulla ethmoidalis superiorly and
uncinate process of ethmoid bone inferiorly
- infundibulum: is a space within the middle
meatus that lies lat to the hiatus it receives the frontonasal duct
(draining the frontal and ant ethmoid sinuses)
- maxillary sinus opens in the middle meatus,
below the bulla and above the inferior edge of the hiatus
- post ethmoidal sinus opens in sup meatus;
nasolacrimal ducts into inf meatus
- sphenoidal sinus opens in sphenoethmoidal
recess
Linings
- vestibule: lined by skin with vibrissae
- roof, adjoining septum and alt wall – olfactory
mucosa
- rest of nasal cavity – respiratory mucosa
- nasal mucosa continuous with that in paranasal
air sinuses
Nerve Supply
- CN I: olfactory area in the upper part of nasal
cavity
- CN V1: ethmoidal branches of
nasocilliary n
- CN V2: branches to the walls of the
nasal cavity
Arterial Supply
- derived mainly from branches of:
- maxillary a.(sphenopalatine, greater palatine)
- ophthalmic a. (ethmoidal a.)
- facial a. (sup labial, ascendimg palatine,
lateral nasal)
Venous drainage
- rich venous plexuses in the nasal mucosa are
drained by pterygoid plexus, facial v and ophthalmic veins
Lymphatics
- drain into submandibular, retropharyngeal, and
upper deep cervical nodes
- definition: they are air filled cavities within the frontal,
ethmoidal, sphenoidal and maxillary bones, are lined with the respiratory
epithelium, and communicate with the nasal cavity through small apertures
- rudimentary at birth; grow at 6-7 years to attain maximum size at
puberty; in adult, they vary considerably in size in different people
Mucosa
- respiratory type, but thin, less vascular and
loosely attached to periosteum
Frontal Sinus
- situated between inner and outer tables of
frontal bones beneath med 1/3 of superciliary arch
- opens into mid meatus via infundibulum
Maxillary Sinus
- is the largest of paranasal sinuses; situated
in maxilla
- pyramidal in shape, apex facing zygoma, and
base towards the nasal cavity
- opens in mid meatus, well above its floor
Ethmoidal
Sinuses
- numerous cavities called cells, within
ethmoidal labyrinth
- are grouped into ant, mid and post groups
- all contained in labyrinthine (lateral) part of
ethmoidal bone
- ant ethmoid sinus opens with frontal sinus in
the middle meatus via infundibulum
- mid ethmoid sinus underlies bulla ethmoidalis;
opens on the bulla into the middle meatus
- post ethmoid opens into sup meatus
Sphenoidal
Sinus
- situated in body of sphenoid bone; divided by a
septum
- related to the pituitary gland, cavernous
sinus, and internal carotid a.
- opens into sphenoethmoidal recess
Nerve Supply of
Paranasal Sinuses
- branches of CN V1
- branches of CN V2
Blood Supply of
Paranasal Sinuses
- branches of maxillary a.
- branches of ophthalmic a.
- branches of facial artery.
Lymphatics of
Paranasal Sinuses
- submandibular group (frontal, ant and middle
ethmoidal and maxillary sinuses)
- retropharyngeal group (post ethmoidal and
sphenoidal sinuses)
- bones that form orbit are lined with periosteum, called periorbita or orbital periosteum
- at optic canal and sup orbital fissure,
periorbita becomes continuous with periosteum lining interior of skull
- also continuous over orbital margins and
through inf orbital fissure with periosteum covering external surface of
skull
- forms funnel-shaped fascial sheath that
encloses orbital contents
- may be easily detached especially from roof and
med wall
Margins of the
orbit
- med: frontal and maxillary
- sup: frontal
- lat: zygomatic and frontal
- inf: zygomatic and maxillary
Walls of the
orbit
- med: maxilla, lacrimal, ethmoid, sphenoid.
Features: nasolacrimal canal, ant & post
- ethmoidal foramen
- sup(roof): frontal (orbital plate), sphenoid
(lesser wing). Features: lacrimal fossa, optic
- foramen, trochlear fossa
- lat: sphenoid (greater wing), zygomatic
(orbital surface). Feature: zygomatic
- canal
- inf (floor): maxilla, zygomatic, palatine.
Features: infraorbital canal and groove
Superior
Orbital Fissure
- separates lat wall from sup wall (roof)
- lies between lesser and greater wings of
sphenoid
- connects orbit with mid cranial fossa
- transmits CN III, IV, V1, ophthalmic
vv.
Inferior
Orbital Fissure
- separates floor from lat wall
- lies between greater wing, maxilla and
zygomatic bone
- connects orbits with pterygolpalatine and
infratemporal fossae
- transmits maxillary n., zygomatic n.,
infraorbital vessels
Contents
Muscles
|
|
Origin |
Insertion |
Innervation |
Action |
|
Levator palpebrae superioris |
roof of orbit, ant to optic canal |
skin of upper eyelid |
CN III |
elevates upper lid |
|
Superior rectus |
common tendinous ring |
just post to sclerocorneal junction |
elevate, adduct |
|
|
Inferior rectus |
depress, adduct |
|||
|
Medial rectus |
adducts eye |
|||
|
Lateral rectus |
CN VI |
abducts eye |
||
|
Superior oblique |
body of sphenoid |
runs through trochlea, post-sup lat orbit |
CN IV |
depress, abduct |
|
Inferior oblique |
maxilla in floor of orbit |
post-inf lat orbit |
CN III |
elevate, abduct |
Fascial Sheath
of eyeball (bulbar fascia or Tenon’s
fascia):
- thin cuplike sheath surrounds eyeball, except
for corneal part
- separates it from fat and or contents in orbit
- attached posteriorly to sclera close to optic
nerve and anteriorly just post to cornea
- tendon of muscles pierce sheath on their way to
their attachments
- blends with fascial sheaths of ocular muscles
- fuses with dural sheath of optic nerve
- potential space between eyeball and fascial
sheath allows eyeball to move freely
- triangular expansions (called check ligaments)
from sheaths of med and lat rectus muscles are attached to lacrimal and
zygomatic bones respectively
- thickening of inf part of the
fascial sheath of eye called suspensory
ligament of eyeball
- suspen lig is attached to ant parts of medal
and lateral walls of orbit
- suspen lig supports eyeball with its
hammock-like shape
Nerves of Orbit
- CN II, III, IV, V1, VI
- ciliary ganglion
Blood Vessels
- orbital contents supplied by ophthalmic a.
- infraorbital a. also contributes some blood to this region
- venous drainage is through ophthalmic vv., sup & inf
Ophthalmic
Artery
- arise from int carotid
a. as it emerges from cavernous sinus
- pass through optic foramen within dural sheath
of optic nerve and runs ant close to
sup-med wall of orbit
- gives off branches to structures in orbit and
to ethmoid bone
Central Artery
of Retina
- one of smallest but most important branches of
ophthalmic a.
- arises inf to optic n.
- runs within dural sheath of optic nerve until
it approaches eyeball, n pierces optic nerve and runs within it to emerge
through optic disc, spreads over int surface of retina
- twigs of artery anastomose with ciliary a. but terminal branches are essentially
end aa.
Ciliary
Arteries
- ciliary aa. supply sclera, choroid, ciliary body and iris
- two long post ciliary
aa. piece sclera and supply ciliary body and iris
- several short post ciliary aa. pierce sclera and supply
choroids
- ant ciliary aa are branches from muscular arteries. They
supply conjunctiva and iris
Lacrimal Artery
- supplies lacrimal gland, conjunctiva and
eyelids
Temporal Fossa
- oval in shape on the lat aspect of the skull
- bounded sup and post by temporal lines
- inf, it communicates with infratemporal fossa
- roofed by temporal fascia
- occupied by temporalis muscle
Infratemporal Fossa
- irregularly-shaped space inf and deep to zygomatic arch and post to
maxilla
- communicates with temporal fossa through interval between arch and
skull and temporal msucles and deep temporal nerves and vessels pass
through it
Boundaries
- ant: post surface of maxilla
- post: styloid process
- sup: infratemporal surface of greater wing of
sphenoid
- inf: continuous with submandibular region
- lat: ramus of mandibular
- med: lat pterygoid plate
Contents
- muscles: lat and med pterygoid, lower part of
temporalis
- nerves: mandibular, otic ganglion, chorda
tympani
- vessels: maxillary a. and v, pterygoid venous
plexus
Maxillary a.
- larger of two terminal branches of ext carotid
- arises post to neck of mandible, passes
forwards (deep to neck), and transverses infratemporal fossa, passes
superf to lat pterygoid and then disappears into pterygopalatine fossa
|
Part
|
Course |
Branches |
|
First |
passes horizontally forwards between neck
of mandible and lower border of pterygoid |
deep auricular ant tympanic mid meningeal accessory meningeal inf alveolar |
|
Second |
runs obliquely forward and upwards superf
to inf head of lat pterygoid |
to muscles of this region |
|
Third |
runs between sup and inf heads of lat
pterygoid, then through pteryggomaxillary fissure into pterygomandibular
fossa |
post sup alveolar infraorbital desc. palantine pharyngeal sphenopalatine |
Pterygoid
Venous Plexus
- is associated with pterygoid muscles
- connected to facial v. through deep facial vv.
- connected to cavernous sinus through vv.
passing through foramen ovale and lacerum
Mandibular
Nerve
- branches into all nerves in infratemporal
region (except for chorda tympani, branch of facial)
- descends through foramen ovale into
infratemporal fossa, divides into sensory and motor fibres
- supply four muscles of mastication, but not
buccinator
|
Part |
Type |
Branch |
|
|
Main trunk |
Motor (3) |
med pterygoid m |
|
|
tensor tympani m |
|
||
|
tensor palati m |
|
||
|
Sensory (1) |
meningeal |
|
|
|
Ant division |
Motor (3) |
massteric n to masseter m |
|
|
deep temporal nn. to temporalis |
|
||
|
n. to lat pterygoid |
|
||
|
Sensory (1) |
buccal |
usually runs between two heads of lat
pterygoid, desc through deep temporalis, supplies skin and mucous membrane of
cheek |
|
|
Post division |
Motor (1) |
n. to mylohyoid and ant digastric |
|
|
Sensory (3) |
auriculotemporal |
encircles med meningeal a., breaks up into
many branches, largest passes post, med to neck of mandible and supplies
auricle and temporal region, also sends articular fibres to temperomandibular
joint |
|
|
lingual |
lies ant to inf alveolar n., sensory to
tongue, floor of mouth and gingivae, enters mouth between med pterygoid
muscle and ramus of mandible, passes ant under oral mucosa, just inf to 3rd
molar tooth chorda tympani branch of facial n. travels
with it |
||
|
inf alveolar |
enters mandibular foramen, passes through
mandibular canal (where it sends nn. to teeth) and appears on face as mental
n., supplies skin and mucous membrane of lower lip, skin of chin |
Otic Ganglion
- is parasympathetic ganglion
- is located in infratemporal fossa, just inf to
foramen ovale, med to mandibular n. and post to med pterygoid muscle
- secretory to parotid gland
Temporomandibular Joint
- type: synovial joint; subtype: modified hinge or condylar variety
- articular surface involved are:
- head or condyle of mandible (inf)
- articular tubercle and mandibular fossa of
squamous temporal bone (sup)
- articular disk separates
joint cavity into sup and inf compartments
- fused with articular capsule surround joint and
is bound sup to limits of temporal articular surface int to neck of
mandible
- articular disc is more firmly attached to
mandible than to the temporal bone
- loose articular capsule attached to
margins of area on temporal bone and neck of mandible
- thickened lat to form lat
(temporomandibular) ligament
- base attached to zygomatic process, apex to lat
side of neck of mandible
- stylomandibular and sphenomandibular also
help to support the T-M joint
|
Movement |
Muscles |
|
depression |
hyoid muscles, gravity |
|
elevation |
temporalis, masseter, med pterygoid |
|
protrusion |
lat and med pterygoid, masseter (deep
fibres) |
|
retraction |
post temporalis |
|
side-to-side |
med and lat pterygoid, masseter |
|
Muscle |
Origin |
Insertion |
|
Temporalis |
temporal fascia |
coronoid process, ant ramus |
|
Masseter |
zygomatic arch |
lat ramus |
|
Lat pterygoid |
sup: infratemporal crest inf: lat lat pterygoid plate |
neck of mandible, articular disk |
|
Med pterygoid |
superf: maxillary tuberosity deep: med lat pterygoid plate |
med ramus |
|
1 |
To what does the term "skull"
refer? |
|
The skeleton of the head, including the
teeth, hyoid bone and ear ossicles. |
|
2 |
What is the skull minus the mandible
called? |
|
The cranium. |
|
3 |
What is the term for the brain case? |
|
The cranium - so some confusion can occur
with the word ‘cranium’. |
|
4 |
What is the rest of the skull called? |
|
The skeleton of the face. |
|
5 |
How many bones are there in the cranium
(brain case)? |
|
Eight. |
|
6 |
Which also contribute to the facial
skeleton? |
|
Sphenoid (by pterygoid process) and
ethmoid. |
|
7 |
What are the junctions between the calvarial
bones called? |
|
Sutures. |
|
8 |
Are they all similar? Which one in
particular is different? |
|
No. The parietotemporal (or squamosal)
suture, which does not interlock. |
|
9 |
Which bone(s) contribute to the anterior
wall of the posterior cranial fossa? |
|
Temporals and occipital. |
|
10 |
Which bone(s) contribute to the anterior
wall of the middle cranial fossa? |
|
Sphenoid. |
|
11 |
Which bone(s) contribute to the anterior
wall of the anterior cranial fossa? |
|
Frontal. |
|
12 |
Which bone(s) contribute to the floor of
the anterior cranial fossa? |
|
Frontal, ethmoid and sphenoid. |
|
13 |
Which bone(s) contribute to the floor of
the middle cranial fossa? |
|
Sphenoid and temporal (both petrous and
squamous parts). |
|
14 |
Which bone(s) contribute to the floor of
the posterior cranial fossa? |
|
Occipital. |
|
15 |
Does the parietal bone contribute to the
lateral wall of the posterior cranial fossa? |
|
Not really. Although there is a deep
groove for the junction of the transverse and sigmoid sinuses, because they
lie in the attached edge of the tentorium the parietal is really excluded
from facing into the posterior cranial fossa. |
|
16 |
What is the pterion? |
|
The REGION where the sphenoid and
parietal bones meet in the temporal region. |
|
17 |
What is the asterion? |
|
The junction of the parietal, occipital
and temporal bones just above and behind the mastoid. |
|
18 |
Where is the bregma? |
|
At the junction of the sagittal and
coronal sutures. |
|
19 |
Where is the lambda? |
|
At the junction of the sagittal and
parieto-occipital (lambdoid) sutures. |
|
20 |
What muscles arise from the calvaria? |
|
The occipitalis and temporalis muscles. |
|
21 |
Which major groups of muscles insert into
the cranial base? |
|
The back muscles - we usually refer to
them as the muscles of the back of the neck. |
|
22 |
What is the diplöe? |
|
The trabecular or cancellous bone forming
the middle layer of the calvarial bones. |
|
23 |
Which is the thicker, the inner table or
the outer table? |
|
Outer. |
|
24 |
Name the main vessel supplying the bones
of the calvaria. |
|
The middle meningeal artery. |
|
25 |
Where does it lie before reaching the
bones? |
|
In the outer layers of the dura. |
|
26 |
Which bone in the skull does it traverse
to enter the cranium? What is the opening it traverses? |
|
The sphenoid, through the foramen
spinosum. |
|
27 |
From what artery does it directly arise?
What vessel gives rise to that artery? |
|
The maxillary, a branch of the external
carotid. |
|
28 |
Where do the veins accompanying the artery
of the calvaria lie? Where do they terminate? |
|
They lie in the dura, accompanying the
meningeal arteries and end in the pterygoid plexus immediately outside the
foramen spinosum. |
|
29 |
About how thick is the dura mater? |
|
˝ - 1 mm. |
|
30 |
What type of tissue is the dura? |
|
Dense, regularly arranged fibrous
connective tissue = aponeurotic tissue. |
|
31 |
What two main roles does the dura service
in the cranium? |
|
As covering of the central nervous system
and as periosteum. |
|
32 |
Which of these roles is not served by the
spinal dura? |
|
The periosteal one, as spinal dura is
separated from bone by extra-dural fat and veins. |
|
33 |
What is the generic term for the venous
blood spaces located in the dura? |
|
The dural venous sinuses. |
|
34 |
Name the venous channel in the attached
border of the falx cerebri. |
|
The superior sagittal sinus. |
|
35 |
Name the venous channel in the attached
border of the tentorium cerebelli. |
|
The transverse (or lateral) sinus. |
|
36 |
What is the name of the intradural space
containing the carotid siphon (internal carotid artery)? |
|
The cavernous sinus. |
|
37 |
Name four other structures found in, or in
the walls of, that space. |
|
III, IV, V and VI nerves. |
|
38 |
What venous channels drain the cavernous
sinus? |
|
The superior and inferior petrosal
sinuses. |
|
39 |
What venous channels drain into the
cavernous sinus? |
|
The ophthalmic veins, the middle
superficial cerebral vein (and the sphenoparietal sinus). |
|
40 |
How is the pituitary gland related to the
cavernous sinuses? |
|
Its lateral poles lie against the medial
walls of the left and right cavernous sinuses. |
|
41 |
What is the tentorium cerebelli? |
|
The low, tent-like dural partition roofing
over the posterior cranial fossa. |
|
42 |
What is the falx cerebri? |
|
The roughly sickle-shaped dural partition
separating the two cerebral hemispheres above the corpus callosum. |
|
43 |
What is the diaphragma sellae? |
|
The dural covering of the pituitary fossa.
A small opening in its centre allows the infundibulum to reach the gland. |
|
44 |
Is there cerebrospinal fluid directly
about the pituitary gland? |
|
No, below the diaphragma sellae the CSF
space is obliterated. |
|
45 |
What direction does the hypophyseal stalk
(infundibulum) run as it passes from the hypothalamus to the pituitary? |
|
It runs downwards and forwards to the
gland. |
|
46 |
Is the arachnoid mater bound to the dura
mater? |
|
No. A smooth walled POTENTIAL space
separates the two layers. |
|
47 |
Is the arachnoid mater connected to the
pia mater? |
|
Yes, by the fine arachnoid processes
crossing the subarachnoid space. |
|
48 |
What is the volume of cerebrospinal fluid? |
|
100 - 150 ml. Production about 500 ml/day. |
|
49 |
About what distance separates pia and
arachnoid? |
|
2 - 3 mm. |
|
50 |
Would you like to have more questions on
the cranium? |
|
|
|
1 |
What is the scalp? |
|
It is the investment of the calvaria. |
|
2 |
What particular characteristic
distinguishes it from the immediately adjacent investing layers? |
|
It has dense fibrous loculated
subcutaneous tissue similar to that of the heel. |
|
3 |
Define its anterior limit. |
|
The eyebrows. |
|
4 |
Define its posterior limit. |
|
The superior muchal lines. |
|
5 |
Where and how does it end at the sides of
the head? |
|
Along the zygomatic arch and just above
the ears, where the much thinned galea blends with the periosteum. |
|
6 |
Does it have distinctive regions? |
|
Yes. Hair bearing and "non-hair"
bearing; (the scalp and forehead of lay terminology). |
|
7 |
What distinguishes such regions? |
|
The presence of terminal hair or its
absence. |
|
8 |
Is that distinguishing feature found
elsewhere in the body? |
|
Yes. Axillary and pubic hair and the beard
and eyelashes and eyebrows are all terminal hair as in the hair on the nape
of the neck. |
|
9 |
How thick is the scalp? |
|
5 mm |
|
10 |
Is it more or less uniformly thick? |
|
It is uniformly thick and of essentially
similar thickness in men and women. |
|
11 |
How thick is the epidermis of the scalp?
Is that thickness about average for epidermis? |
|
100 m. Yes, that is average for
the body. |
|
12 |
How thick is the subcutaneous layer of the
scalp? How does that compare with the average thickness throughout the body? |
|
1.5 mm. Yes, that is thickness over most
of the body. |
|
13 |
Mention THREE distinctive features of the
scalp (or of major parts of the scalp). |
|
A Terminal Hair B Loculated
subcutaneous tissue C Muscle
superficial to the investing fascia |
|
14 |
With what other parts of the body does it
share feature A? |
|
Face (in males), Axilla, Pubic and
perianal areas, eye brows and eyelids. |
|
15 |
With what other parts of the body does it
share feature B? |
|
The palms of the hands and soles of the
feet. |
|
16 |
With what other parts of the body does it
share feature C? |
|
The face, front of neck and upper chest.
(The Dartos muscle in the scrotum is smooth muscle). |
|
17 |
What are the dimensions of Frontalis
approximately? |
|
5 cm x 5 cm |
|
18 |
From what does Frontalis arise? In to what
does it insert? |
|
The Galea aponeurotica; the skin of the
eyebrows. |
|
19 |
How big is Occipitalis in comparison to
Frontalis? |
|
Much smaller. |
|
20 |
Does occipitalis abut the midline on each
side? |
|
No. |
|
21 |
What are the auricular muscles? |
|
Three superficial muscle slips running
from the galea to the cartilage of the external ear near the cartilaginous
external auditory meatus. |
|
22 |
What is the Temporoparietalis muscle? |
|
A fairly extensive sheet of muscle in the
upper temporal region running from the ear upwards and forwards to the galea. |
|
23 |
What is the name given to the Frontalis,
Occipitalis, Temporoparietalis and galea aponeurotica together? |
|
Epicranins muscle. |
|
24 |
At which layer does the scalp move on the
cranium? |
|
At the layer of loose connective tissue
between galea and periosteum (layer 4). |
|
25 |
Where is the galea aponeurotica firmly
attached to bone? |
|
At the nuchal line (and, because it is
much thinner, less firmly to the zygomatic arches). |
|
26 |
What layers and structures separate the
epidermis in the temporal region from the parietal and sphenoid bones? |
|
Dermis, thinned galea, rather denser layer
4 (loose connective tissue), the temporalis fascia (representing a true
investing fascia), the temporalis muscle and periosteum. |
|
27 |
What vessels supply the scalp? |
|
The supraorbital (medial and lateral
branches). superficial temporal and occipital (assisted by the supratrochlear
and posterior auricular). |
|
28 |
Which of them come from the internal
carotid artery? Are they direct branches of the internal carotid? |
|
A supraorbitals and supratrochlear. No,
they are branches of the ophthalmic a. |
|
29 |
Which of them come from the external
carotid artery? Are they direct branches of the external carotid? |
|
The superficial temporal, occipital (and
posterior auricular) are direct branches of the external carotid. |
|
30 |
How much of the scalp is supplied by
branches of the ophthalmic artery? |
|
Just the forehead region. (The
corresponding nerves (the supraorbital) supply right back to the vertex). |
|
31 |
Which arteries anastomose across the
sagittal suture? |
|
The superficial temporals (thereby
limiting the territory of the supraorbital arteries). |
|
32 |
What veins drain the scalp? |
|
Veins running with and having the same
names as the arteries. |
|
33 |
Which drain to the internal jugular vein?
How? |
|
The superficial temporals (thereby
limiting the territory of the supraorbital arteries). |
|
34 |
Which drain into the external jugular
vein? |
|
The occipital, posterior auricular and
superficial temporal. |
|
35 |
What nerves supply the scalp? |
|
Cranial nerve V and cervical nerve 2. |
|
36 |
What parts are supplied by cervical
nerves? |
|
The occipital region up to the vertex. |
|
37 |
What parts are supplied by cranial nerves?
Which cranial nerve? |
|
The forehead back to the vertex and the
temporal regions. Cranial nerve V, the trigeminal. |
|
38 |
Which major division of the 5th cranial
nerve supplies skin of the temporal region? |
|
The mandibular division mainly (with a
small contribution from the maxillary division anteriorly). |
|
39 |
How are the muscles of the scalp
innervated? |
|
By the VIIth cranial nerve (facial nerve). |
|
40 |
Are there lymphatics in the scalp? |
|
Yes. |
|
41 |
Where are lymph nodes found close to the
scalp? What are the names of the various groups? |
|
Around its lower limits, laterally and
posteriorly. Preauricular, mastoid and occipital groups. |
|
42 |
Haemorrhage from the veins piercing the
cranial vault (from, for instance, moulding of the skull during birth) is
limited to the extent of a single cranial bone. Why? |
|
Because the periosteum is bound down
tightly at the sutures and this type of bleeding occurs between the
periosteum and the particular bone. |
|
43 |
Gashes to the scalp bleed freely. Why? How
would you control the bleeding? |
|
Because the arteries are large and are
tethered in the dense connective tissue of the scalp. Moderate pressure where
the arteries enter the scalp. |
|
44 |
Infections of sebaceous glands in the
scalp are very painful. Why? |
|
Because the pus is unable to spread far in
the subcutaneous tissue and pressure builds up. |
|
45 |
Cuts in scalp in a coronal direction gape;
those in a sagittal direction don’t. Why? |
|
Because the tension in the galea is from
front to back because of the way the muscles are arranged. |
|
46 |
Is the scalp well nourished? |
|
Extremely well. |
|
47 |
Do the bald areas of scalp contain hair
follicles?; sebaceous glands? sweat glands? |
|
Yes. Yes. Yes. |
|
48 |
Is there hair on the forehead? If so, what
kind? |
|
Yes. Normal fine body hair. |
|
49 |
Are eyebrow hairs different from head
hair? |
|
No. Both are terminal hair. |
|
50 |
Do you think you have learned enough about
the scalp? |
|
|
|
1 |
What is the posterior limit of the face? |
|
The coronal plane immediately behind the
rami of the mandible and in front of the vertebral column (plane C) and in
the upper 3 cm the plane through the anterior surface of the sphenoid
(plane B). |
|
2 |
What is the upper limit of the face? in
anatomy? in lay terms? |
|
The eyebrows. The hairline. |
|
3 |
What is the lower limit of the face? |
|
The floor of the mouth. |
|
4 |
Name the reference blocks comprising the
face. |
|
Orbital, maxillary, dental; upper nasal,
lower nasal, buccal, pharyngeal and pterygoid. |
|
5 |
Name the three principal areas of contact
between the face and the cranium. |
|
The frontomaxillary sutures; the
frontozygomtic sutures; the pterygopalatine sutures (where, in effect, the
body of the maxilla is supported from behind by the pterygoid process). |
|
6 |
What parts of the face have particularly
thin skin? |
|
The eyelids (and the external ears, if we
include them in the face). |
|
7 |
How much thinner than average is (i) the
epidermis and (ii) the dermis in these areas? |
|
Both epidermis and dermis are half the
usual thickness (that is, in the eyelids they are about 50 m
and 600 m respectively). |
|
8 |
How thick and dense is the subcutaneous
tissue in these regions? |
|
In the eyelids very thin and delicate with
litte fat. (The subcataneous layer is absent in the pinna except in the
lobes). |
|
9 |
How thick are the lips? |
|
12 mm. |
|
10 |
How thick are the cheeks? |
|
12 mm. |
|
11 |
Does the skin or subcutaneous tissue
contribute most to the thicknesses? |
|
The subcutaneous layer is 9 - 10 mm thick. |
|
12 |
How is the extent of the lips defined? |
|
They are the area where the skin if FIRMLY
bound to the deeper tissues. |
|
13 |
Are there external markings indicating the
extent of the lips? |
|
The nasolabial folds and labiomental fold
(mental = of the chin). |
|
14 |
What particular change in the firmness of
skin attachment occurs on passing from the lips to the cheeks? |
|
The skin becomes somewhat more mobile in
the cheeks, but not as free in the front of the neck, for instance. |
|
15 |
Is the beard different in principal from
head hair? |
|
No; both are terminal hair with follicles
extending into the subcutaneous layer. |
|
16 |
How much denser is the hair follicle
population on the face (and scalp and neck) than elsewhere on the body? |
|
10 x. |
|
17 |
How much denser are the hairs on these
parts than elsewhere? |
|
About 3 x (many follices are
"resting" in a cycle measured in years). |
|
18 |
Are sweat glands more profuse on the face
(and scalp and neck) than elsewhere on the body? why? |
|
At least twice as dense. The head and neck
are the principal sites of heat loss. Hands next, then feet. |
|
19 |
What layer of tissue represents the investing
fascia in the face? |
|
The periosteum of the bones of the face. |
|
20 |
Is the mucosa of the gums facing the
vestibule of the mouth superficial or deep to the investing fascia? |
|
Superficial. |
|
21 |
In what layer do the muscles of facial
expression lie? |
|
In the deep half of the subcutaneous
tissue. |
|
22 |
What is the posterior limit of this muscle
group? |
|
The nuchal lines on the occiptal bone. |
|
23 |
What is the anterior (actually inferior)
limit of this group? |
|
The chest for a few centimetres below the
clavicle; (platysma extends to this level). |
|
24 |
What is the name of the muscle surrounding
and contained in the eyelids? |
|
Orbicularis oculi. |
|
25 |
What is its action? |
|
It blinks the eyelids and more forcibly,
screws them tight shut. |
|
26 |
What is the name of the muscle surrounding
the mouth? |
|
Orbicularis oris. |
|
27 |
What is its action? |
|
It purses the lips. |
|
28 |
Where do your find the Buccinator muscle? |
|
In the cheeks, posterior to orbicularis
oris. |
|
29 |
Is it a muscle of facial expression? |
|
Yes. |
|
30 |
What muscles arise from the zygomatic
bone? |
|
Zygomaticus major and z. minor passing
down into the upper lip. |
|
31 |
What muscles arise just below the
infraorbital margin of the maxilla? |
|
Levator labii superious and levator labii
superious alaeque nasi (alaeque = and also of the). |
|
32 |
Where does the Levator anguli oris arise? |
|
From the anterior surface of the maxilla BELOW
the infraorbital canal. |
|
33 |
Why is there no "Levator labii
inferioris?" |
|
The orbicularis oris opposes the depressor
of the lower lip. These are ELEVATORS of UPPER lip and DEPRESSORS
of LOWER lip. |
|
34 |
Locate Risorius, Procerus and Corrugator
supercilii muscles. |
|
At angle of mouth, between eyebrows and
under inner end of eyebrows. |
|
35 |
Can you name any other muscles in the
face? |
|
Compressor naris, Mentalis, Depressor
anguli oris, Platysma. |
|
36 |
Describe the extent of Platysma. |
|
From corner of mouth to upper chest. |
|
37 |
From which vessel does the facial artery
arise? |
|
The external carotid artery. |
|
38 |
Is the first part of its course
superficial or deep to the mandible? |
|
Deep. |
|
39 |
Where does it cross the lower border of
the mandible? |
|
Immediately in front of the Masseter
muscle. |
|
40 |
What is the inner canthus of the eye? |
|
The inner angle where the two eyelids
meet. |
|
41 |
In its course to the inner canthus does
the facial artery run superficial to, deep to or in amongst the muscles of
facial expression? |
|
Amongst. |
|
42 |
Name its branches arising near the angle
of the mouth. |
|
The superior and inferior labial arteries. |
|
43 |
Where does the facial vein terminate? Does
it ever lie deep to the mandible? |
|
In the internal jugular vein (usually
having coalesced with the lingual vein). No. |
|
44 |
Name three separate groups of lymph nodes
in the face. |
|
Parotid, submandibular; mental. |
|
45 |
To which group do the outer parts of the
eyelids mainly drain? |
|
Parotid. |
|
46 |
To which group do the inner parts of the
eyelids mainly drain? |
|
Submandibular. |
|
47 |
To which group does the upper lip mainly
drain? |
|
Submandibular. |
|
48 |
To which group does the lower lip mainly
drain? |
|
Mental. |
|
49 |
Which nerve is sensory to the upper
eyelid? |
|
Ophthalmic division of trigeminal (V1). |
|
50 |
Which nerve is sensory to the lower
eyelid? |
|
Maxillary division of trigeminal (V2). |
|
51 |
Which nerve is sensory to the upper lip? |
|
Maxillary, V2. |
|
52 |
Which nerve is sensory to the lower lip? |
|
Mandibular divisiion of trigeminal V3. |
|
53 |
Which nerve is sensory to the dorsum
("leading edge") of the nose? |
|
The external nasal branch of V1 (via
anterior ethmoidal). |
|
54 |
Which nerve is motor to the muscles of
facial expression? |
|
Facial nerve (VII). |
|
55 |
Do you think that that is enough
questioning about the face? |
|
|
|
1 |
Which bones contribute to the roof of the
orbit? |
|
Frontal, sphenoid. |
|
2 |
Which bones contribute to the floor of the
orbit? |
|
Maxilla, Zygomatic (and palatine). |
|
3 |
Which bones contribute to the medial wall
of the orbit? |
|
Maxilla (frontal process), lacrimal,
ethmoid and sphenoid. |
|
4 |
Which bones contribute to the lateral wall
of the orbit? |
|
Sphenoid and Zygomatic. |
|
5 |
What bony elements bound the superior
orbital fissure? |
|
Greater and lesser wings and body of
sphenoid. |
|
6 |
What bony elements bound the inferior
orbital fissure? |
|
Great wing of sphenoids, zygomatic,
maxilla and body of sphenoid. |
|
7 |
Which bones bound the bony nasolacrimal
canal? |
|
Lacrimal, maxilla and inferior concha. |
|
8 |
What bony elements bound the optic canal? |
|
The root of lesser wing and body of
sphenoid. |
|
9 |
What is the diameter of the eye ball? |
|
24 mm. |
|
10 |
In which part of the orbit does the
eyeball lie? |
|
In the anterior half (of its length). |
|
11 |
How closely does it approach the orbital
walls? |
|
To within 6 mm. |
|
12 |
What is the bulbar fascia or Tenon’s
capsule? |
|
The connective tissue lining of the
fibrofatty socket for the eye. |
|
13 |
About which point does the eyeball move? |
|
Its centre. |
|
14 |
Name the two major refracting elements of
the eye. |
|
The cornea and lens. |
|
15 |
What medium surrounds the iris? |
|
Aqueous humour. |
|
16 |
What medium surrounds the optic nerve? |
|
Cerebrospinal fluid. |
|
17 |
Where is the dura attached to the eyeball? |
|
Immediately medial to the posterior pole. |
|
18 |
Where do most of the nerves and arteries
enter the eyeball? |
|
Immediately about the dural sheath of
N.II. |
|
19 |
To what bony elements is the fibrous
annulus (of Zinn) attached? |
|
The body, lesser wing and, by a small area,
the great wing of the sphenoid. |
|
20 |
In what direction does teh superior rectus
muscle run? |
|
Fowards and laterally, at an angle of 22˝°
to sagittal plane. |
|
21 |
In which quadrant of the eyeball does the
superior oblique muscle insert? |
|
Postero-supero-lateral quadrant. |
|
22 |
Where does the inferior oblique muscle
arise? |
|
Immediately lateral to the nasolacrimal
canal. |
|
23 |
Where does it insert? |
|
Into the horizontal meridian immediately
lateral to the posterior pole of the eye. |
|
24 |
Which muscle is innervated by the 4th
cranial nerve? by the 6th cranial nerve? |
|
The superior oblique; the lateral rectus. |
|
25 |
How long approximately are the rectus
muscles? How wide? |
|
40 mm; 10 mm. |
|
26 |
Name three nerves lying between the
orbital roof and the fibrous annulus. |
|
Lacrimal, frontal and trochlear nerves. |
|
27 |
Name three nerves passing through the
fibrous annulus. Which one of these has divided into two divisions? |
|
Oculomotor, masociliary and abducens
nerves. The oculomotor is divided. |
|
28 |
Briefly describe the course of the
ophthalmic artery. |
|
Through optic canal, along lateral side of
optic nerve, over nerve at midpoint to medial wall, then forwards. |
|
29 |
Which nerve follows essentially the same
course? |
|
The nasociliary nerve (but enters orbit
through superior orbital fissure). |
|
30 |
Where is the ciliary ganglion located? |
|
Just lateral to optic nerve, several
millimeters behind the eye. |
|
31 |
What type of neurons does it contain? |
|
Parasympathetic post-ganglionic neurons. |
|
32 |
What structures does it supply? |
|
The smooth muscle of the ciliary body and
iris. |
|
33 |
What type of tissue fills the interstices
of the orbital cavity? |
|
Delicate fibrofatty tissue. |
|
34 |
Name the firm connective tissue structures
forming the basis of the eyelids. |
|
The tarsal plates. |
|
35 |
What covers the deep surface of these
structures? |
|
Conjunctiva. |
|
36 |
What muscle is found in the eyelids? |
|
Orbicularis oculi + levator palpebrae
superiorus. |
|
37 |
How many rows of eyelashes are present in
each lid? |
|
Two or three. |
|
38 |
Where are the tarsal (Meibomian) glands
situated? |
|
In deep grooves in the tarsal plates. |
|
39 |
At what level does the upper lid lie in
relation to this iris and pupil? At what level does the lower lid lie? |
|
Between the top of iris and top of pupil.
Just at the bottom of the ribs. |
|
40 |
What is the vertical and horizontal extent
of the conjunctival sac? |
|
About 30 mm each way. |
|
41 |
Name the structure about which the
lacrimal gland is folded or clamped? |
|
The tendon of the levator palpebrae
superioris. |
|
42 |
Do ducts arise from both parts? |
|
Yes. |
|
43 |
Where do these ducts open? |
|
Into the lateral half of the superior
conjunctival fornix. |
|
44 |
Where are the puncta of the lacrimal ducts
located? |
|
At the medial end of the rows of
eyelashes. |
|
45 |
Where do the lacrimal ducts run? |
|
Within the substance of the medial
palpebral ligament. |
|
46 |
Where does the lacrimal sac lie? |
|
In the fossa formed by the lacrimal bone
and frontal process of the maxilla. |
|
47 |
What is the direction of the lateral
palpebral ligament? |
|
Forwards from the orbital margin. |
|
48 |
To what bony structure is the medial
palpebral ligament attached? |
|
Over an area several mm in diameter on the
frontal process of the maxilla. |
|
49 |
Set your own question and answer it. |
|
|
|
1 |
Which reference planes bound the mouth? |
|
3, 4, A, B and R (each side) |
|
2 |
Which reference planes bound the buccal
cavity? |
|
3, 4, A, B, and P (each side) |
|
3 |
What are the functions of the mouth? |
|
Food and liquid intake; accessory air
intake; articulation in speech; (investigating environment). |
|
4 |
Which muscles forms the foundation of the
cheek? |
|
Buccinator. |
|
5 |
What is its nerve supply? |
|
The facial (VIIth) nerve. |
|
6 |
Which muscle forms the foundation of the
lips? |
|
Orbicularis oris. |
|
7 |
About how thick are the lips and cheeks? |
|
12 mm |
|
8 |
What type of epithelium is found on the
mucosa of the mouth? |
|
Non-keratinizing stratified squamous
epithelium. |
|
9 |
What is the name of the region of the
mouth bounded by the lips and cheeks on the one hand and the teeth and gums
on the other? |
|
Vesibule of the mouth. |
|
10 |
What is the name of the region of the
mouth bounded by the tongue on the one hand and the lower teeth and gums on
the other? |
|
Linguo-alveolar groove. |
|
11 |
Which bones contribute to the hard palate? |
|
Maxilla and palatine. |
|
12 |
Name the five major bony elements of the mandible
(three are bilateral). |
|
Head, coronoid process, ramus, body and
alveolar process. |
|
13 |
Name the four types of teeth in the adult
dentition. |
|
Incisors, canines, premolars and molars. |
|
14 |
Which belong to the "anterior
teeth"? |
|
Incisors and canines. |
|
15 |
Which belong to the "cheek
teeth"? |
|
Premolars and molars. |
|
16 |
How many roots on an upper permanent
molar? What are their positions? |
|
3; lingual, mesiobuccal and distobuccal. |
|
17 |
How many roots on a lower molar? What are
their positions? |
|
2; mesial and distal. |
|
18 |
Which nerves supply the upper cheek teeth? |
|
The posterior superior alveolar nerves (2
or 3). |
|
19 |
Which nerve supplies the mucous membrane
of the gum immediately lateral to the upper molars? |
|
One of the posterior alveolar nerves
(which doesn’t supply teeth). |
|
20 |
Briefly describe the course of the nerve
supplying the upper incisors and canine. |
|
It curves downwards and medially from
infraorbital nerve in anterior face of maxilla, passing just below the
opening of the nose. |
|
21 |
Which nerve supplies the gum immediately
lateral to the lower molars? |
|
The buccal nerve. |
|
22 |
Which nerve supplies the mucosa of the
part of the vestibule related to the lower anterior teeth? |
|
The mental nerve. |
|
23 |
Which nerve supplies the skin of the lower
lip and chin? |
|
The mental nerve. |
|
24 |
Which nerve supplies the skin of the upper
lip and the related mucous membrane? |
|
The infraorbital nerve. |
|
25 |
Which nerve supplies the mucosa of the
roof of the mouth (hard palate)? |
|
The greater palatine nerve. |
|
26 |
Which nerve supplies the mucosa of the
floor of the mouth including that of the buccal part (anterior two-thirds) of
the tongue? |
|
The lingual nerve. |
|
27 |
Which artery supplies the hard palate? |
|
The greater palatine artery. |
|
28 |
Which artery supplies the floor of the mouth? |
|
The lingual artery. |
|
29 |
Which arteries supply the upper teeth? |
|
The superior alveolar arteries. |
|
30 |
Which artery supplies the lower teeth? |
|
The inferior alveolar artery. |
|
31 |
Where does that artery arise? |
|
From the maxillary artery in the pterygoid
region. |
|
32 |
Which lymph nodes receive lymph from the
mouth? |
|
Retropharyngeal, submandibular and
submental. |
|
33 |
Name the nerve supplying the muscles of
the tongue. |
|
Hypoglossal (Cranial nerve XII). |
|
34 |
Where does it arise? |
|
From the anterior aspect of the medulla. |
|
35 |
How does it leave the cranium? |
|
Through the hypoglossal (anterior
condylar) canal. |
|
36 |
How low does it descend in the neck? |
|
To the level of the great horn of the
hyoid bone. |
|
37 |
What special features are there of the
mucosa of the dorsum of the tongue? |
|
Papillae. |
|
38 |
Is there a submucosa in the tongue? |
|
No. |
|
39 |
Which salivary gland opens into the
vestibule? |
|
The parotid. |
|
40 |
Which salivary glands open into the buccal
cavity? |
|
The submandibular and sublingual glands. |
|
41 |
Which gland has its duct opening near the
second upper molar tooth? |
|
The parotid. |
|
42 |
Which gland has its duct opening below and
behind the medial lower incisor? |
|
The submandibular. |
|
43 |
Which salivary gland has little mucus in
its secretion? |
|
The parotid. |
|
44 |
What muscle forms the floor of the mouth? |
|
The mylohyoid. |
|
45 |
Where does its nerve supply arise? |
|
From the inferior alveolar nerve. |
|
46 |
Which other muscles lie in the floor of
the mouth? |
|
The anterior belly of digastric; the
geniohyoid. |
|
47 |
From which embryological structure does
the floor of the mouth arise? |
|
The mandibular (1st) arch. |
|
48 |
From which embryological structure does
the roof of the mouth arise? |
|
The maxillary process of the mandibular
arch. |
|
49 |
Into which region does the mouth open
posteriorly? |
|
The isthmus of the fauces (of the
pharynx). |
|
50 |
Do you require any further questions on
the mouth? |
|
|
|
1 |
Name the planes bounding the lower nasal
block. |
|
2, 3, A, B, and P (on each side). |
|
2 |
Which bones enclose the olfactory part of
the nose? |
|
The ethmoid, with sphenoid behind and
maxilla and nasal bones in front. |
|
3 |
Name the bones contributing to the
external nose. |
|
Nasal bones and maxillae. |
|
4 |
Name two major cartilages of the external
nose. |
|
Lateral nasal (from septal) and greater alar
cartilage. |
|
5 |
What is the name of the region immediately
inside the nostril? |
|
The vestibule of the nose. |
|
6 |
Which bones contribute to the nasal
septum? |
|
Ethmoid and vomer. |
|
7 |
What other component contributes to the
skeleton of the nasal septum? |
|
The septal cartilage. |
|
8 |
Which is the largest nerve on the septum?
Where does it end? |
|
The nasopalatine; on the incisive pad. |
|
9 |
About how wide (from medial to lateral) is
the frontal sinus? |
|
30 mm |
|
10 |
In which part(s) of the frontal bone does
it lie? |
|
In the squama (underlying the forehead)
and in the orbital plate. |
|
11 |
Where does it open into the nose? |
|
Into the anterior part of the infundibulum
(c.60%) or immediately in front of it into middle meatus (c.40%). |
|
12 |
Which is the longest meatus? |
|
The inferior. |
|
13 |
Which is the shortest? |
|
The superior (or supreme meatus if
present). |
|
14 |
What structure forms the lower part of the
lateral wall of the middle meatus? |
|
The uncinate process. |
|
15 |
What structure forms the upper part? |
|
The bulla. |
|
16 |
Name the gap between these two. |
|
The hiatus semilunaris. |
|
17 |
Where do the posterior ethmoidal air cells
open? |
|
Into the superior meatus. |
|
18 |
What do we call the region on each side
from which the sphenoidal air sinus opens. |
|
The sphenoethmoidal recess. |
|
19 |
Which is the most voluminous paranasal air
sinus? |
|
The maxillary sinus. |
|
20 |
Where does it communicate with the nose? |
|
In the infundibulum. |
|
21 |
What structures traverse the cribriform
plate? |
|
The olfactory nerves and the anterior
ethmoidal nerve and vessels. |
|
22 |
Name the cranial nerve supplying the nose? |
|
The trigeminal. |
|
23 |
Which area does its first division supply? |
|
The external nose. |
|
24 |
What is the extent of the olfactory
sensory area? |
|
Over the superior and much of middle
concha and opposing parts of septum. |
|
25 |
Name the branch of the maxillary artery
supplying the nose. |
|
The sphenopalatine artery. |
|
26 |
Name the nerves supplying the superior and
middle conchae. |
|
The posterior superior lateral nasal
nerves. |
|
27 |
What type of epithelium lines the nasal
cavity (except the lower vestibule)? |
|
Respiratory epithelium. |
|
28 |
Describe the nature of the nasal mucosa. |
|
Thick and vascular, with many glands. |
|
29 |
Which nerves supply skin of the external
nose? |
|
The external nasal branch of the anterior
ethmoidal nerve; the infractrochlear; and the external nasal branches of the
infraorbital nerve. |
|
30 |
Which of them supply skin inside the
nostril? |
|
Those of the infraorbital nerve. |
|
31 |
What areas of the nose are supplied by the
anterior superior alveolar nerve? |
|
Small areas on the lateral and septal
walls at the anterior end of the inferior concha and the floor between. |
|
32 |
What supports the mucosa of the lateral
wall of the choanal part of the nose? |
|
The medial pterygoid plate. |
|
33 |
Which reference planes bound the choanal part
of the nose in front, and above? |
|
Plane B and Plane 2. |
|
34 |
Which nerves supply this part of the nose? |
|
The posterior nasal branches of the
pterygopalatine ganglion. |
|
35 |
To what structures are the lateral nasal
cartilages attached? |
|
They are continuous with the septal
cartilage and are firmly attached to the nasal bones and the frontal process
of the maxilla. |
Aortic Arch Derivatives:
1st: part of MAXillary artery
2nd: stapedial artery and hyoid artery
3rd: Common carotid artery and proximal internal
carotid
4th: on left, aortic arch; on right, proximal right
subclavian
6th: proximal part of pulmonary arteries and ductus
arteriosus
1st arch is MAXimal
Second
= Stapedial
C is third letter of the alphabet
4th arch (4 limbs) = systemic
6th arch = pulmonary and pulmonary-to-systemic shunt
(ductus arteriosus)
Mastication Muscles (all innervated
by V3):
- Masseter, teMporalis, Medial
pterygoid (these close jaw)
- lateral pterygoid (this is the only one that
lowers)
- In summary, M's munch. Lateral Lowers.
Palat muscles:
All muscles with palat in their name (except tensor
veli palatini via CN V) are innervated by CN X. [Explained in branchial stuff
below]
Glossus muscles:
All muscles with glossus in their name (except
palatoglossus via CN X) are innervated by CN XII. [Also explained below]
Carotid Sheath:
You've seen it before: VAN
- Internal Jugular vein (lateral)
- Common carotid (medial)
- Vagus Nerve (posterior)
Branchial Stuff (with
mnemonics):
Branchial Clefts derived from
ectoderm
Branchial Arches derived from mesoderm and neural
crest
Branchial Pouches derived from endoderm
CAP covers from outside to
inside: Cleft = ecto, Arch = meso, Pouch = endo
Arches (mesoderm):
Branchial arch 1 derivatives:
(lots of M's)
Meckel's cartilage: Mandible, Malleus, incus, sphenoMandibular ligament
Muscles:
Muscles of Mastication (temporalis, Masseter, lateral and Medial pterygoids),
Mylohyoid, anterior belly of digastric, tensor tympani, tensor veli palatini
Nerve: CN V3
(V2 also involved)
Branchial arch 2 derivatives:
(lots of S's)
Reichert's cartilage: Stapes, Styloid process, leSSer horn of hyoid, Stylohyoid
ligament
Muscles:
muscles of Silly facial expression, Stapedius, Stylohyoid, poSterior belly of
digastric
Nerve: CN VII
Branchial arch 3 derivatives:
(This is the easiest one)
Cartilage:
greater horn of hyoid
Muscle:
stylopharyngeus
Nerve: CN IX
(think of pharynx - stylopharyngeus innervated by glossopharyngeal
nerve)
Branchial arch
Cartilage:
thyroid, cricoid, arytenoid, corniculate, cuneiform
Muscle:
pharyngeal constrictors, cricothyroid, levator veli palatini, intrinsic muscles
of larynx, trapezius, SCM (See note below)
Nerve: 4th
arch - CN X, 6th arch - recurrent laryngeal branch of X (See note below
about XI)
Note: All of the intrinsic muscles of larynx
innervated by the inferior laryngeal nerve of CN X (a continuation of the
recurrent laryngeal nerve) EXCEPT the cricothyroid muscle, innervated by
external branch of the superior laryngeal nerve (branch of CN X). The
cricothyroid specifically comes from the 4th arch, and that is why it has
separate nerve innervation than the intrinsic laryngeal muscles which come
specifically from the 6th arch. But if asked on an exam, just group all of
these muscles into 4th-6th arch.
Note: When we talk about arch 4 and 6, it is acceptable to lump everything
together into one big group: 4-6. You will see in your green notes that X and
XI are nerves of the 4th-6th arch. Technically speaking, the accessory fibers
of XI are the motor fibers that are carried by the vagus to the muscles of the
larynx. So, when asked about the nerve of the 4th - 6th arch, just say X(XI).
See p 180 green notes, Netter 121.
Note: Branchial Arch 5 makes no developmental
contributions.
Summary:
Arch 1: V2, V3
Arch 2: VII
Arch 3: IX
Arch 4, 6: X(XI)
Note: This is the simplest way to conceptualize
head/neck muscle innervation. Actually, this is analogous to
compartmentalization of the limbs.
Clefts (ectoderm):
1st cleft: external auditory
meatus
2nd - 4th clefts: temporary cervical sinuses,
obliterated ultimately by 2nd arch mesenchyme
Note: Persistent cervical sinus can lead to
branchial cyst in the neck
Pouches (endoderm):
1st pouch: middle ear cavity,
eustachian tube, mastoid air cells (endoderm lined structures of the ear)
2nd pouch: palatine tonsil epithelium
3rd pouch: inferior parathyroids (from dorsal wings),
thymus (from ventral wings)
4th pouch: superior parathyroids
5th pouch: ultimobranchial bodies - This is where a
subset of neural crest cells migrate to ultimately become the C cells of the
thyroid (calcitonin producing cells, part of the neuroendocrine system
-HISTOLOGY correlation)
"Mnemonic": 3rd pouch: 3 structures - thymus, Left
and Right inferior Parathyroids
Pretrematics:
Remember that each arch has a
cranial nerve (discussed above)
There are pretrematic branches of these nerves that
"invade" the arch right before it.
1. Ophthalmic division of V1
leaves V2 and V3 behind in the first arch and associates with the optic cup in
front of the first arch (gives us tactile sensation to the eye)
2. A pretrematic from arch 2
(VII territory) invades arch 1 (V3 territory). This is the chorda tympani (VII)
which joins the lingual nerve (V3) and gives us taste.
3. A pretrematic from arch 3 (IX
territory) invades arch 2 (VII territory). This is the tympanic nerve (IX)
which provides sensory innervation to the middle ear and auditory tube. Also
remember the tympanic plexus which is a mix of VII and IX nerves (Netter 117,
119)
Cervical Plexus / Ansa
Cervicalis (Netter 27)
Plexus divided into muscular and
cutaneous branches
Cutaneous (C2-3): Great auricular, lesser occipital,
transverse cervical nerves
Cutaneous (C3-4): Supraclavicular nerves
Motor: Ansa Cervicalis (C1-3) - innervates
infrahyoid (strap) muscles of the neck; and Phrenic nerve (C3-5)
Muscles innervated by ansa
(C1-3):
-geniohyoid
(C1 via hypoglossal nerve)
-thyrohyoid (C1
via hypoglossal nerve; remember that XII travels right on top of the ansa - the
superior root of the ansa is actually called the descendens hypoglossi) These
are the only two hyoids innervated by C1 via XII.
-sternothyroid (C1-3)
-sternohyoid (C1-3)
-omohyoid (C1-3)
What hyoid muscles are not
innervated by the ansa?
- mylohyoid (1st arch, V3)
- stylohyoid (2nd arch VII (cervical branch))
Thyroid Stuff:
Thyroid develops from the
thyroid diverticulum which forms in the floor of the foregut (no branchial
pouches involved), descends into neck.
Connected to tongue by
thyroglossal duct - disappears and becomes foramen cecum
Most common ectopic thyroid site
is tongue
Tongue Stuff:
Anterior 2/3 formed from 1st
branchial arch. Therefore, tactile sensation via V3, taste via VII. (The chorda
tympani joins lingual nerve).
Posterior 1/3 formed from 3rd and 4th arches.
Therefore, sensation and taste mostly via IX, most posterior via X.
All motor from XII.
Cleft Lip/Palate:
Cleft lip - failure of fusion of
maxillary and medial nasal processes
Cleft palate - failure of fusion of lateral palatine
processes, nasal septum, and/or median palatine process
Larynx:
7 muscles you need to know:
Cricothyroid - stretch and tense vocal cord (only
muscle innervated by external laryngeal n.)
Posterior Cricoarytenoid - (only muscle to ABduct vocal cord)
Lateral Cricoarytenoid - ADduct vocal fold
Thyroarytenoid
- relax vocal fold
Vocalis
(formed from thyroarytenoid) - alters fold during phonation
Oblique arytenoid - close inlet
Transverse arytenoid - close inlet (oblique and transverse perform same task)
Motor: All muscles except
cricothyroid (external branch of superior laryngeal n.) innervated by recurrent
laryngeal n. All X(XI).
Sensory: The internal branch of the superior
laryngeal nerve will receive sensory information above the vocal fold where the
recurrent will receive sensory info below the folds.
Parasympathetics and
Ganglia:
The important take home point: the
trigeminal nerve acts as a carrier for parasympathetic fibers from III, VII,
IX. The trigeminal itself contains no inherent parasympathetic activity.
The major function of parasympathetics in
the head is to act as secretomotor to the lacrimal gland, salivary glands, and
mucus glands of the oral and nasal cavities and sinuses. It will increase
secretion.
VII (Netter 117):
The origin of parasympathetic fibers in VII comes from the nervus
intermedius. It merges with the facial nerve at the sensory geniculate
ganglion. The greater petrosal nerve continues on and merges with the deep
petrosal nerve (totally sympathetic, postganglionic coming off the carotid
plexus) in the pterygoid canal to form the vidian nerve. The
vidian nerve enters the pterygopalatine ganglion and parasympathetics
synapse. Postganglionic autonomics exit the fossa via V2 through five exits
(listed below) to get to the mucus glands of nose and palate, and lacrimal
gland.
Two entrances of the Pterygopalatine
Fossa:
Pterygoid Canal (vidian nerve)
Entrance of maxillary nerve through foramen rotundum
Five Exits of the Pterygopalatine Fossa:
Sphenopalatine foramen - (nasal branches of V2 going to nasal cavity)
Greater palatine foramen - (greater palatine n. of V2 going to hard palate)
Lesser palatine foramen - (lesser palatine n. of V2 going to soft palate)
Inferior orbital fissure - (zygomatic n. of V2 going to lacrimal gland)
Palatovaginal canal - (pharyngeal branch of V2 going to nasopharynx)
Cranial Nerve Lesions:
VII Lesion (Bell's Palsy) -
cannot operate muscles of facial expression. Affected muscles on same side of
lesion
X lesion - Ask to say "Ah" - uvula will
point away from lesion
XI lesion - head will be turned toward lesion (SCM
action)
XII lesion - stick out tongue - tongue will point to
lesion
Cranial Foramina:
Know the foramina for all of the
cranial nerves. In addition, know the stylomastoid foramen, petrotympanic
fissure, and foramen spinosum and their contents.
Clinical Correlations:
I suspect a patient is faking neck injury.
How can I tell?
- Most patients do not know about the function of the
SCM. The contralateral muscle turns the head away from it. First. ask the
patient to shrug his/her shoulders (trapezius, XI). Say for example the patient
cannot shrug the left shoulder. Ask the patient to turn his/her head left or
right (SCM, XI) If the patient says he/she has trouble turning the head to the
left, the person is faking. If he/she cannot turn it to the right, the injury
is probably real.
What are some significant
features of the carotid bifurcation?
- Location of the carotid body
- an oxygen chemoreceptor - sensory info carried back to CNS via CN IX, X
- Location of carotid sinus - a
pressure receptor - sensory info carried to CNS via CN IX, X
- Place where clots can form
(think turbulent flow). Performing a bilateral carotid massage on an older
patient may actually throw emboli into the circle of Willis. A lot of good your
anastomoses are going to do in this situation...
What would be the clinical
presentation of a patient with bilateral recurrent laryngeal nerve damage?
- Acute dyspnea - the vocal
muscles have stretched and tensed from unopposed cricothyroid, closing off the
airway.
What structure must I puncture
in a tracheotomy?
- Cricothyroid ligament
What are three symptoms from
evulsed T1 (besides clawhand)
- ptosis
- miosis
- anhydrosis
Why does both a sympathetic and
parasympathetic lesion to the eye cause ptosis?
- levator palpebrae superioris (skeletal muscle -
innervated by CN III)
- tarsal or Mueller's muscle (smooth muscle - innervated
by sympathetics)
Questions:
1. Which of the following
courses through the jugular foramen?
A. CN VII
B. inferior sagittal sinus
C. middle meningeal artery
D. straight sinus
E. CN X
2. The chorda tympani branch of
CN VII carries:
A. motor fibers to the stapedius
muscle
B. parasympathetic fibers to the parotid gland
C. sensation from the tympanic membrane
D. taste from the anterior two-thirds of the tongue
E. taste from the posterior one-third of the tongue
3. Sensory innervation of the
larynx is by branches from the
A. CN V
B. CN VII
C. CN VIII
D. CN IX
E. CN X
4. In a patient with an aneurysm
of the aortic arch associated with hoarseness, one would immediately look for
paralysis of the left:
A. anterior belly of the
digastric muscle
B. cricothyroid muscle
C. posterior belly of the digastric muscle
D. posterior cricoarytenoid muscle
E. omohyoid muscle
5. Following a blow to the side
of the head, extradural hemorrhage is usually caused by bleeding from the:
A. cavernous sinus
B. emissary veins (connections between intracranial
sinuses and external veins)
C. middle cerebral artery
D. middle meningeal vessels
E. superior sagittal sinus
6. A patient with Bell Palsy
(paralysis of CN VII) experiences food collecting in his oral vestibule.
Paralysis of which muscle is most likely causing this muscle?
A. buccinator
B. masseter
C. mentalis
D. orbicularis oris
E. zygomaticus major
7. Pain impulses from the tip of
the tongue would most likely be carried to neurons in which of the following
ganglia?
A. geniculate
B. otic
C. pterygopalatine
D. superior vagal
E. trigeminal
8. Each of the following nerves
supplies muscle derived from the branchial arches EXCEPT the
A. VII
B. IX
C. XII
D. V
E. X
9. Congenital absence of the
parathyroids is most likely accompanied by absence or poor development of the
A. lungs
B. Anterior pituitary
C. thyroid gland
D. nasopharyngeal portions of the eustachian tube
E. thymus
10. Endoderm contributes to the
formation of each of the following EXCEPT the
A. eustachian tube
B. liver
C. parathyroid glands
D. tooth enamel
E. trachea
11. In a newborn, obstruction of
the pharynx caused by a large mass in the posterior third of the tongue is most
likely a result of
A. branchial cyst
B. ectopic parathyroid tissue
C. ectopic thymic tissue
D. ectopic thyroid tissue
E. hypertrophied lymphoid tissue
12-14. Mechanisms involved in
swallowing:
A. Closure of nasopharynx from
oropharynx
B. Depression of the larynx and hypopharynx to
produce negative pressure in the pharynx
C. Elevation of the larynx and hypopharynx
D. Movement of a bolus of food posteriorly into
oropharynx
E. Protection of the airway
12. Styloglossus muscle
13. Tensor veli palatini and
superior constrictor muscles
14. Stylohyoid and digastric
muscles
Questions with more than one
answer:
15. A fracture of the cribriform
plates that tears the meninges is likely ot result in
A. loss of sense of smell
B. rupture of nasolacrimal duct
C. leakage of CSF into nasal cavity
D. injury to maxillary division of CN V
16. The nerve supply of the
tongue is derived, in part, from the nerve of the:
A. First branchial arch (V3)
B. Second arch (VII)
C. Third arch (IX)
D. Fourth arch (X)
17. The first branchial arch
contributes to the formation of the:
A. malleus and incus
B. maxilla and mandible
C. muscles of mastication
D. muscles of facial expression
18. The intermaxillary segment
of the developing upper jaw contributes to the formation of:
A. Philthrum of the lip
B. Primary or anterior palate
C. Premaxillary part of the maxilla
D. Posterior or secondary palate