\

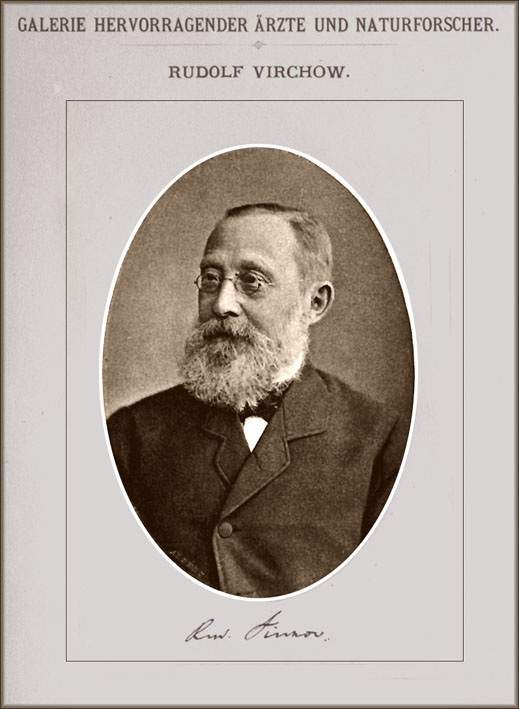
Father of pathology
Rudolf Ludwig Karl Virchow
1821 - 1902
Rudolf Ludwig Karl Virchow was among the greatest minds in medicine in the 19th century. As a result of his hard work and determination, great strides were made in the fields of pathological and physiological medicine. Virchow was born in Schivelbein, Pomeranian, Prussia on October 13, 1821. He attended Friederich Wilheim Institute where he studied to become a physician with a passion for pathological histology.
Throughout his studies, Rudolf Virchow also performed a plethora of research disproving that phlebitis was the cause of most diseases. Once he graduated from Friederich Wilheim Institute, Virchow went on to study at the University of Berlin where he became a medical doctor in 1843 .
He was employed as an intern at Charite Hospital in Berlin but was suspended on March 31, 1849 due to his liberal view of the German government. He was championed as the founder of cellular pathology because of his extensive research that disease is created and reproduced at the cellular level of the body. However, he did not accept Pasteur's germ theory, and in later life devoted himself to archaeology and anthropology, forming a close friendship with Schliemann and collaborating in the excavation of Troy.
Rudolf Virchow was not only a brilliant physician and researcher but he was a father and husband as well. In 1850 he married Rose Mayer and throughout their marriage they became parents of 6 children, three sons and three daughters .
Rudolf Virchow was always busy attempting to better the lives of the German people. Even at the time of his death on September 5, 1902 in Berlin, Rudolf Virchow was still serving on committees and counsels and working diligently as editor of journals in medical education . He was constantly working to provide quality health care to his patients and fighting for the their rights with the German Government

born on December 27, 1822 in Dole, in the region of Jura, France. His discovery that most infectious diseases are caused by germs, known as the "germ theory of disease", is one of the most important in medical history.
His work became the foundation for the science of microbiology, and a cornerstone of modern medicine.
Pasteur's phenomenal contributions to microbiology and medicine can be summarized as follows. First, he championed changes in hospital practices to minimize the spread of disease by microbes. Second, he discovered that weakened forms of a microbe could be used as an immunization against more virulent forms of the microbe. Third, Pasteur found that rabies was transmitted by agents so small they could not be seen under a microscope, thus revealing the world of viruses. As a result he developed techniques to vaccinate dogs against rabies, and to treat humans bitten by rabid dogs. And fourth, Pasteur developed "pasteurization", a process by which harmful microbes in perishable food products are destroyed using heat, without destroying the food.
Louis Pasteur discovered the method for the attenuation of virulent microorganisms that is the basis of vaccination. He developed vaccines against chicken cholera, anthrax and swine erysipelas. After mastering his method of vaccination, he applied this concept to rabies. On July 6, 1885, Pasteur tested his pioneering rabies treatment on man for the first time : the young Joseph Meister was saved.
Carl Rokitansky (1804 – 1878)
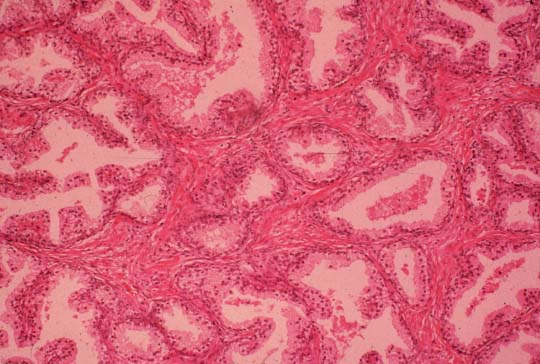
Investigation of the pathology of the CNS lesions continued throughout the 19th century, with developments in microscope technology allowing the analysis to become increasingly detailed.
This slide shows a portrait of Carl Rokitansky, one of the most outstanding morphological pathologists of the 19th century. Working at the Institute of Pathology in Vienna,
he was one of the first to examine MS lesions microscopically .
Rokitansky made a particularly important observation
in 1857 when he noticed 'fatty corpuscles' in the MS lesions. Charcot later described these as:
"the wreck and detritus resulting from the disintegration of the nerve-tubes
Penicillin researchers (c1940)
During the 1950s, James Gowans revealed the life cycle of the lymphocyte, whose role was at that time completely obscure. Gowans showed that the small lymphocyte continuously recirculated from the blood to the lymph and back again to the blood. He later demonstrated that this cell was at the centre of the immunological response.

James Gowans
History of the Microscope
The Development of the Microscope
(Janssen / circa 1590’s)
Although the original microscope was a rather simple device, its ability to magnify the range of human vision paved the way for a revolutionary discovery of microbial life. Credit for the initial device has historically been given to a Dutch craftsman, Zacharias Janssen, working in the Netherlands late in the 16th century as a spectacle maker. These tradesmen, considered to be the world’s finest, had been using concave lenses for more than a century to correct far-sightedness. Janssen subsequently extrapolated this approach to visual amplification by creatively attaching two such lenses at opposite ends of hand-held tube. Janssen’s device was unquestionably primitive, but the microscope (from Greek words meaning "to see small"), would shortly reveal a hitherto unimagined realm of life.
http://www.az-microscope.on.ca/
From ancient times, man has wanted to see things far smaller than could be perceived with the naked eye.
This led to the construction, in the 16th century, of a magnifier composed of a single convex lens, and this, in turn, led to the eventual development of the microscope
Perhaps the most famous early pioneers in the history of the microscope are Digges of England and Hans and Zcharias Janssen of Holland
But it was Antony van Leeuwenhoek who became the first man to make and use a real microscope.
Leeuwenhoek ground and polished a small glass ball into a lens with a magnification of 270X, and used this lens to make the world's first practical microscope
Because it had only one lens, Leeuwenhoek's microscope is now referred to as a single-lens microscope. Its convex glass lens was attached to a metal holder and was focused using screws.
After his historic invention, Leeuwenhoek continued to devote himself to studies base on the microscope. His discoveries included bacteria, bellanimalcules and spermatoza. Leeuwenhoek actually constructed a total of 400 microscopes during his prolific lifetime
The magnification ratio of a single-lens microscope like the one invented by Leeuwenhoek is calculated in the same way as calculations are made for a simple magnifying glass.
250mm--accepted to be the distance of most distinct vision--is divided by the length of the lens.
To increase the power of a single-lens microscope, the focal length has to be reduced. However, a reduction in focal length necessitates a reduction of the lens diameter, and after a point, the lens becomes difficult to see through
To solve this problem, the compound microscope system was invented in the seventeenth century. This type of microscope incorporates more than one lens so that the image magnified by one lens can be further magnified by another
day, the term "microscope" is generally used to refer to this type of compound microscop
in the compound microscope, the lens closer to the object to be viewed is refers to as the "objective", while the lens closer to the eye is called the "eyepiece"
Since its invention, the compound microscope has made tremendous contributions to the progress of science. Using a compound microscope that he had built himself, the 17th-century Englishman Robert Hooke discovered the fact that living things are composed of cells
n the medical world, Louis Pasteur of France used a compound microscope to discover yeast fungus, while Karl J. Ebert, a German bacteriologist, employed a compound microscope in his discovery of Eberthella Thyphosa
It was also a compound microscope that Robert Koch discover tubercle and cholera bacilli
The 19th century saw dramatic progress in the development of the microscope, thanks to the contributions of such great minds as Carl Zeiss, who devoted significant effort to the manufacture of microscopes, Ernst Abbe, who carried out a theoretical study of optical principles, and Otto Schott, who conducted research on optical glass



MD4 SUMMER 2013 ONE OF THE BEST

DANIL HAMMOUDI.MD

 Hoping YOU WILL LEARN SOMETHING AND
HAVE FUN
Hoping YOU WILL LEARN SOMETHING AND
HAVE FUN



MOST OF THE LECTURE ARE PASS PROTECTED
Lectures are below the pictures so scroll down






I will not post on Moodle beside grades and syllabus.
If you have trouble accessing these lecture, see the powerpoint in the library.
This website is in a constant update
Healthy is merely the slowest possible rate at which one can die.




|
In the 60's, people took acid to make the world weird. Now the world is weird and people take Prozac to make it normal.
SOME GENERAL DEFINITION PATHOLOGY The branch of medical science that studies the causes and nature and effects of diseases therefore pathology will not mean autopsy but other as biopsy of tissue to know what is going on , cytology as papsmears in one word anything that will be seen under microscope after tissue removal [surgery] is part of the pathology. Agood surgeon should be a good pathologist in understanding the disease and pathway.
DISEASE: any departure from a state of health ANATOMIC PATHOLOGY: tissues and organs CLINICAL PATHOLOGY: blood and other body fluids FORENSIC PATHOLOGY: the application of the science and methods of pathology to the resolution of problems of the law and issues of public interest
do you think a biopsy or FNA is needed Thyroid wasn't even described in scientific literature until in 1656 Thomas Wharton made a distinction between it and the larynx, but for 200 more years its function (regulation of the body's metabolism) was completely unknown. Goiters are excessive enlargements of the thyroid, which may be caused by iodine deficiency, or by an excess of thyroid stimulating hormone. Because we salt everything with iodized salt, iodine deficiency is never a problem in America, but it is elsewhere in the world. ---------------------------------------------------------------------
Guideline to hCG levels during pregnancy:hCG levels in weeks from LMP (gestational age): Guideline to Progesterone levels during pregnancy:•
1-28 ng/ml Mid Luteal Phase (Average is over 10 for
un-medicated cycles and over 15 with medication use)
===============================
|
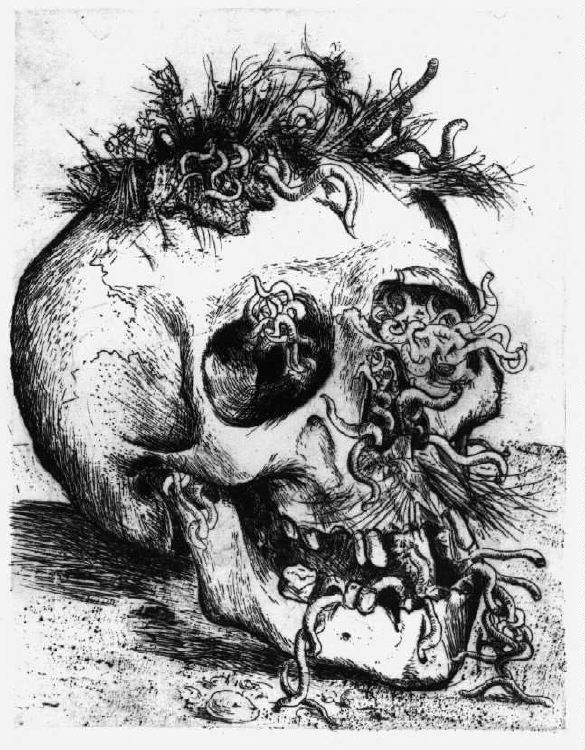
MEDICOLEGAL SCENE INVESTIGATION
1) rigor mortis:
2) livor mortis:(discoloration)
3) algor mortis:
IMMUNOHISTOCHEMISTRY Immunohistochemical methods are based on immunoenzimatic reactions using antibodies (mono or polyclonal) to detect cell or tissue antigens, Several possibilities exist of visualizing such interactions, by using different enzymes (peroxidase, alkaline phosphatase, etc.) or different cromogens (DAB, AEC, Fast RED, etc.). TYPES OF DEATHS REQUIRING
NOTIFICATION OF
|

Rembrandt Harmenszoon van Rijn
(1606-1669):
The Anatomy Lecture of Dr. Nicolaas Tulp (1593-1674) in
1632
The pathologist usually has the last word in medicine,
because he does the autopsy. He tells everyone else what the correct diagnosis should have been and why the treatments didn't work.
He can also be the ace in the hole for a malpractice defense attorney, and the secret weapon of the plaintiff's attorney.
the pathologist is one that knows everything but to late
surgeon is the guy that knows and act
internist is the guy that knows nothing and cook to get the answer

![]()
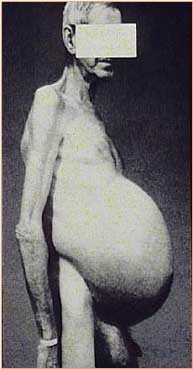
ASCITES

HERPES
APOPTOSIS
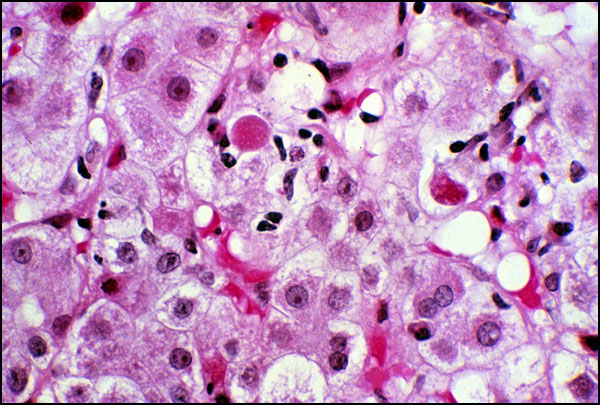
congestive hepatomegaly

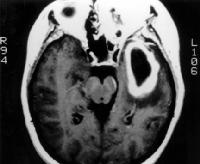
BRAIN ABSCESS

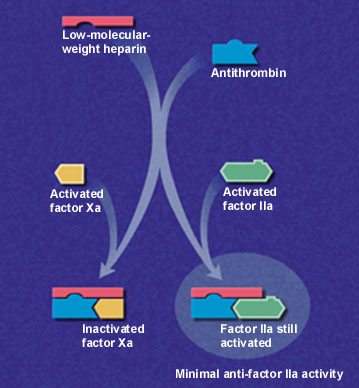
DVT
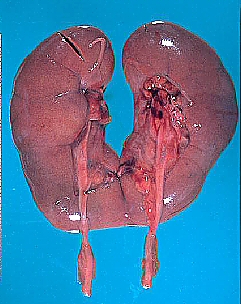
HORSESHOE KIDNEY
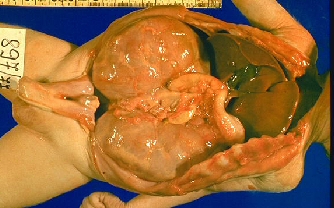
POLYCYSTIC KIDNEY [CONGENITAL]
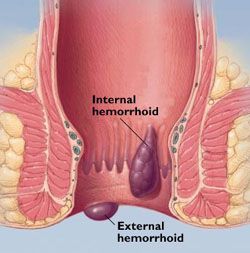
PROSTATE HYPERPLASIA

TREPANATION
|
Seeking
a snapshot of historic human cancer rates over seven
millennia, a team of archaeologists and medics
examined 3,160 skeletons in a collection at the
Croatian Academy of Sciences and Arts. Above, a
femur, or thigh bone, shows signs of a benign tumor
around the joint.
|


collegiate power lifting championships at Penn State. The unfortunate competitor, who expressed a plea to remain anonymous, remembered to surgeons that he was " stuck" at the bottom of a personal best attempt in the squat lift when he "sort of pulled his stomach in and pushed extra hard, at the same time as trying to complete the lift."
He remembers a loud popping, splattering noise then a fierce stabbing pain and then not being able to move from the squat position. He remained in this position for about half an hour, since trying to stand caused him overwhelming agonizing pain. Paramedics arrived and applied anesthesia on the spot and carried him to an ambulance. He was rushed to surgery, where surgeons described the trauma as an explosive and aggravated prolapse of the bowel". Meanwhile it was revealed that the weight was removed from his shoulders at the time of the incident by two "spotters" on either side of the lifter. The third spotter who was standing behind the lifter was unfortunately sprayed with fecal matter at the time of the incident. This spotter promptly fainted when he realized the extent of of the injury to the lifter, who was a personal friend.
This compounded the task of first aid officers who were at a loss as to how to treat the injury to the lifter in any case, who remained in the squatting position moaning in pain much to the consternation of the helpless audience. The hapless lifter had successful surgery to relieve the prolapse, but remained immobilized with his feet elevated in stirrups for 2 weeks to ensure "internal compliance with the surgery and that the organs retracted successfully".
To add insult to injury, the ex-lifter required rectal stitching to partially occlude the anal orifice and stitch the rectal passage (which had significantly expanded and torn during the prolapse) and also was put on a low fiber low residue diet to combat flatulence to avoid any possibility of a recurrence. [rotten.com]



Morbid Obesity
Avicenna [985-1037]
Avicenna, b. 980, Bukhara, Iran d. 1037, Hamadan Arabic IBN SINA, in full ABU 'ALI AL-HUSAYN IBN 'ABD ALLAH IBN SINA, Iranian physician, the most famous and influential of the philosopher-scientists of Islam. He was particularly noted for his contributions in the fields of Aristotelian philosophy and medicine.
He composed the Kitab ash-shifa' ("Book of Healing"), a vast philosophical and scientific encyclopaedia, and the Canon of Medicine, which is among the most famous books in the history of medicine.
Albertus Magnus [1193-1280]
Roger Bacon [1220- 1292] Thomas Aquinas [1225-1274]
Arnold de Villanova [1240 -1310?]
Nicolas Flamel [1330-1418] Geber [14th century]
Basil Valentine [supposed 15th cent.] The 12 Keys Georg Agricola [1494-1555] Paracelsus [1493-1541] Jacob Bohmen [1575 - 16?] Valentin Weigel >[1533-1588]
John Dee [1527-1608] Edward Kelley [1555-1595] Jacob Boehme [1575-1624] Heinrich Khunrath [1560-1605]
Jan Baptista van Helmont [1577-1644]
Robert Boyle [1626-1691] Isaac Newton [1642 -1727] Count Cagliostro [1743-1795]
Count de Saint Germain [18th Century]
Demosthenes - The Alchemist God Alexandre Saint Yves d'Alveydre - Archeometre [19th Century]
|
REJECTION ACTIVITY INDEX (RAI) |
||
|---|---|---|
|
Criteria which can be used to score liver allograft biopsies with acute rejection, as defined by the World Gastroenterology Consensus Document. |
||
|
Category |
Criteria |
Score |
|
Portal Inflammation |
Mostly lymphocytic inflammation involving, but not noticeably expanding, a minority of the triads |
|
|
Expansion of most or all of the triads, by a mixed infiltrate containing lymphocytes with occasional blasts, neutrophils and eosinophils |
||
|
Marked expansion of most or all of the triads by a mixed infiltrate containing numerous blasts and eosinophils with inflammatory spillover into the periportal parenchyma |
||
|
Bile Duct Inflammation Damage |
A minority of the ducts are cuffed and infiltrated by inflammatory cells and show only mild reactive changes such as increased nuclear:cytoplasmic ratio of the epithelial cells |
|
|
Most or all of the ducts infiltrated by inflammatory cells. More than an occasional duct shows degenerative changes such as nuclear pleomorphism, disordered polarity and cytoplasmic vacuolization of the epithelium |
||
|
As above for 2, with most or all of the ducts showing degenerative changes or focal lumenal disruption |
||
|
Venous Endothelial Inflammation |
Subendothelial lymphocytic infiltration involving some, but not a majority of the portal and/or hepatic venules |
|
|
Subendothelial infiltration involving most or all of the portal and/or hepatic venules |
||
|
As above for 2, with moderate or severe perivenular inflammation that extends into the perivenular parenchyma and is associated with perivenular hepatocyte necrosis |
||
|
Total RAI Score = _/9 |
||
|
Reference Anonymous. Banff Schema for Grading Liver Allograft Rejection: An International Consensus Document.Hepatology 1997;25(3):658-63. University of Pittsburgh. |
||